PCOS stands for Polycystic Ovarian Syndrome, but the weird thing is that usually the person does not have even one cyst on their ovaries. PCOS is really more of a collection of symptoms, which originally was thought to only occur with cysts on the ovaries, hence the name.
PCOS is actually really common, affecting around 4% of all women. (1) PCOS can severely impact the quality of a person’s life, and it can increase the risk of infertility. Luckily, most of the time the symptoms are easy enough to catch, and there are some good natural treatment options that have proven success.
What are the symptoms of PCOS?
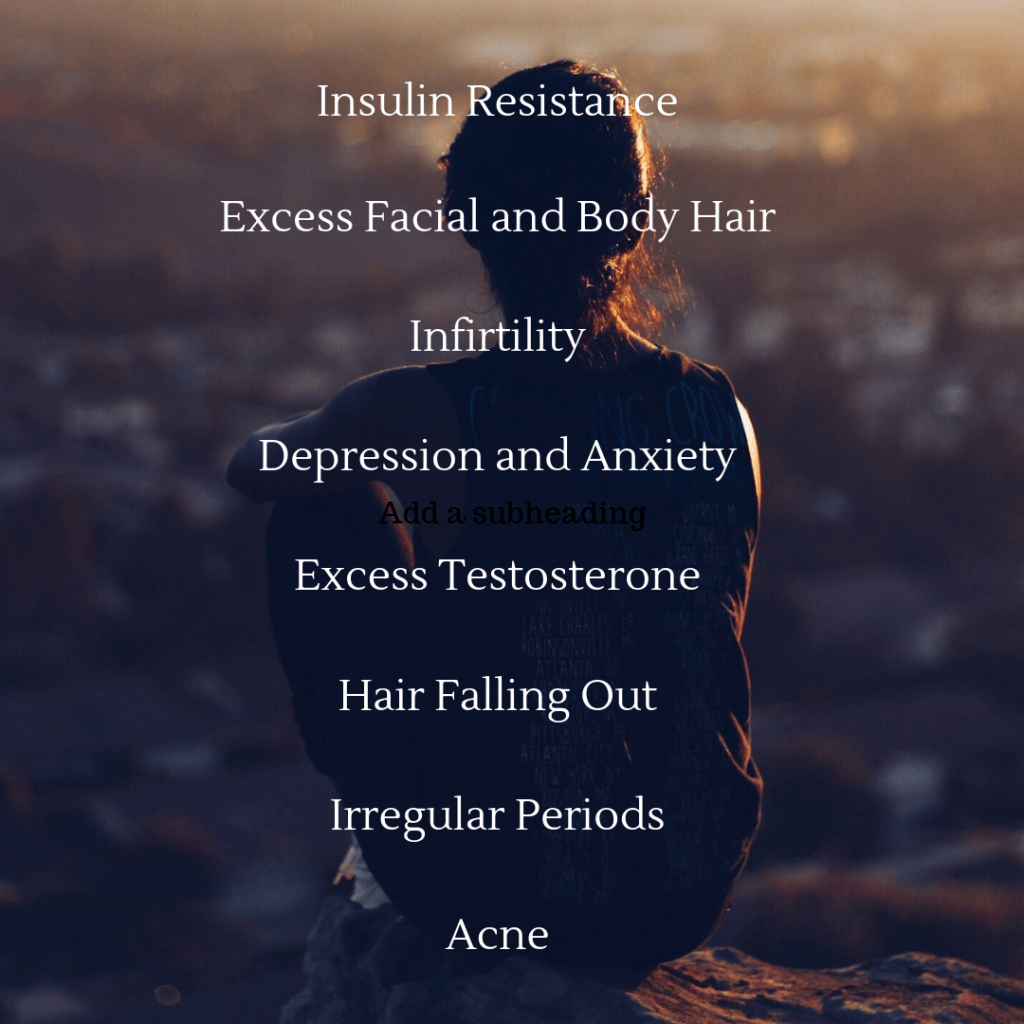
While the exact features can differ from person to person, the usual symptoms of PCOS are the following:
- Insulin resistance
- Unwanted excess body or facial hair
- Too much testosterone or androgens
- Altered ovarian function causing skipped, missed, delayed, or light or heavy periods
- Excess body fat, especially around the waist (not always but common)
- Increased risk factors for cardiovascular disease
- Oily skin and prone to acne
- Depression and low mood, and sometimes anxiety (14)
- Loss of hair
- Increased risk of hormonal cancers, such as breast and endometrial cancer (5)
What Causes PCOS?
What we do know is that insulin resistance is intimately tied to PCOS. (2) This may also help explain the obesity link, as obesity greatly increases the risk for insulin resistance.
This insulin resistance also likely contributes to the increased levels of androgens, including testosterone, that characterize the syndrome.
These high levels of androgens can: (3)
- Interfere with the signals for ovulation
- Cause the follicles in the ovaries to enlarge, forming cysts
- Contribute to the excess body and facial hair growth, as well as the oily skin and acne
So now you can see that the cysts are really an “effect”, not the “cause” of the symptoms. Since PCOS is very likely on a spectrum – with some people having the full-blown syndrome and some barely being classified as having PCOS – we can understand that although some medical doctors still use the number of cysts as part of the diagnosis, the cysts do not really have to be there to benefit from treating this collection of symptoms.
Besides insulin resistance and high levels of androgens as causes, you can also be at an increased risk if there are people in your family that have PCOS, as there are genetic links. (4)
Diet for PCOS
The ideal diet for someone with PCOS would be similar to the ideal diet for someone with insulin resistance or Type 2 Diabetes, as insulin resistance is such a prominent feature.
Dietary changes can be simple, but can have a large influence. It has been shown that simply achieving a 5% drop in bodyweight, if overweight, can lead to a large decrease in insulin resistance, outside of other dietary changes. (5)
Setting up a diet in a way that will help reduce insulin resistance and thus help with PCOS symptoms include: (5, 9)
- Limited refined sugars such as table sugar, soda, candy, and even fruit juices
– Unrefined sugars coming from whole, unaltered fruits are okay and encouraged (6) - Limiting animal fats (including butter), trans fats, fried foods, and refined vegetable oils (soybean, corn, palm, etc.)
– Extra virgin olive oil (from a trusted brand) and *unrefined* coconut oil are great oils to use instead (7) - Limiting refined carbohydrates like pasta, white bread, white rice, etc.
– Whole grain foods like oats, quinoa, beans and lentils, and all-bran cereals are much better options - Choosing stevia over Splenda (i.e. sucralose) (8)
- Eating generous amounts of vegetables and tubers like sweet potatoes
- Making sure you are eating enough high quality protein
Effect of Exercise on PCOS
Exercise has been shown to play a big role in helping to reduce the symptoms of PCOS, including decreasing insulin resistance, waist circumference, and overall fitness levels. (10)
Moreover, one study found that aerobic exercise improved the morphology of their ovaries even without changes in weight or fat loss. (11)
The women in this study completed 16 weeks of individualized aerobic exercise training 5 times per week under supervision on a treadmill for about 30-60 min per day.
The women with PCOS started the study with larger ovaries and more follicles than the control group who did not have PCOS (despite having a similar body composition).
After the 16 weeks, the PCOS group became more insulin sensitive, had a small drop in testosterone levels, and had less ovarian follicles, though still higher than the control group. They did not lose any weight, likely due to eating more to make up for the exercise, and weight loss would have likely made the results stronger according to previous research.
Personally, a combination of slow aerobic training, higher intensity interval training, and resistance training would likely be best in my opinion. Resistance training is very beneficial for insulin resistance. This is because while endurance training makes the existing muscles more likely to suck up glucose, resistance training increases the overall muscle mass to suck up more glucose from the bloodstream. (12, 13)
Supplementation for PCOS
There has actually been a large amount of research done into the effects of various supplements on the symptoms of PCOS.
In the next article in this series, I will be reviewing the evidence of one particularly important supplement to ease PCOS symptoms. Stay tuned!
Please post any questions or comments below!
References
- Guzick DS. Polycystic ovary syndrome. Obstet Gynecol. 2004 Jan;103(1):181-93. Review. Apr;103(4):799. PubMed PMID: 14704263.
- Dunaif A. Insulin resistance and the polycystic ovary syndrome: mechaxnism and implications for pathogenesis. Endocr Rev. 1997 Dec;18(6):774-800. Review. PubMed PMID: 9408743.
- https://www.nichd.nih.gov/health/topics/pcos/conditioninfo/causes
- Unluturk U, Harmanci A, Kocaefe C, Yildiz BO. The Genetic Basis of the Polycystic Ovary Syndrome: A Literature Review Including Discussion of PPAR-gamma. PPAR Res. 2007;2007:49109. doi:10.1155/2007/49109
- Faghfoori Z, Fazelian S, Shadnoush M, Goodarzi R. Nutritional management in women with polycystic ovary syndrome: A review study. Diabetes Metab Syndr. 2017 Nov;11 Suppl 1:S429-S432. doi: 10.1016/j.dsx.2017.03.030. Epub 2017 Apr 5. Review. PubMed PMID: 28416368.
- Sharma SP, Chung HJ, Kim HJ, Hong ST. Paradoxical Effects of Fruit on Obesity. Nutrients. 2016;8(10):633. Published 2016 Oct 14. doi:10.3390/nu8100633
- Khaw KT, Sharp SJ, Finikarides L, et al. Randomised trial of coconut oil, olive oil or butter on blood lipids and other cardiovascular risk factors in healthy men and women. BMJ Open. 2018;8(3):e020167. Published 2018 Mar 6. doi:10.1136/bmjopen-2017-020167
- Romo-Romo A, Aguilar-Salinas CA, Brito-Córdova GX, Gómez-Díaz RA, Almeda-Valdes P. Sucralose decreases insulin sensitivity in healthy subjects: a randomized controlled trial. Am J Clin Nutr. 2018 Sep 1;108(3):485-491. doi: 10.1093/ajcn/nqy152. PubMed PMID: 30535090.
- Moran LJ, Ko H, Misso M, Marsh K, Noakes M, Talbot M, Frearson M, Thondan M, Stepto N, Teede HJ. Dietary composition in the treatment of polycystic ovary syndrome: a systematic review to inform evidence-based guidelines. J Acad Nutr Diet. 2013 Apr;113(4):520-45. doi: 10.1016/j.jand.2012.11.018. Epub 2013 Feb 16. Review. PubMed PMID: 23420000.
- Kite C, Lahart IM, Afzal I, et al. Exercise, or exercise and diet for the management of polycystic ovary syndrome: a systematic review and meta-analysis. Syst Rev. 2019;8(1):51. Published 2019 Feb 12. doi:10.1186/s13643-019-0962-3
- Redman LM, Elkind-Hirsch K, Ravussin E. Aerobic exercise in women with polycystic ovary syndrome improves ovarian morphology independent of changes in body composition. Fertil Steril. 2011;95(8):2696–2699. doi:10.1016/j.fertnstert.2011.01.137
- Poehlman ET, Dvorak RV, DeNino WF, Brochu M, Ades PA. Effects of resistance training and endurance training on insulin sensitivity in nonobese, young women: a controlled randomized trial. J Clin Endocrinol Metab. 2000 Jul;85(7):2463-8. PubMed PMID: 10902794.
- Shaibi GQ, Cruz ML, Ball GD, Weigensberg MJ, Salem GJ, Crespo NC, Goran MI. Effects of resistance training on insulin sensitivity in overweight Latino adolescent males. Med Sci Sports Exerc. 2006 Jul;38(7):1208-15. PubMed PMID: 16826016.
- Chaudhari AP, Mazumdar K, Mehta PD. Anxiety, Depression, and Quality of Life in Women with Polycystic Ovarian Syndrome. Indian J Psychol Med. 2018;40(3):239–246. doi:10.4103/IJPSYM.IJPSYM_561_17
49 Comments
Kimberly · February 23, 2024 at 12:37 am
Where is the next article about the important supplement?
horizonsmaroc.com · May 17, 2025 at 9:42 pm
Es steuert und beeinflusst eine Vielzahl wichtiger Prozesse
im Körper – übrigens auch bei Frauen. Die durchschnittlichen Blutwerte gesunder Männer liegen nach der Pubertät zwischen zwölf und 30 Nanomol Testosteron pro Liter.
Mangelt es ihnen an dem Geschlechtshormon, bekommen sie das empfindlich zu
spüren. Sie fühlen sich schlapp und antriebslos,
sind niedergeschlagen, leiden womöglich sogar unter Blutarmut.
Kreditkartenzahlungen werden über die Deep Web Portal
Ltd abgewickelt. Bei Fragen zu deinem Test oder den Ergebnissen sind wir jederzeit persönlich für dich da.
Sicher, unkompliziert und mit fachkundigen Empfehlungen helfen wir dir, dein Wohlbefinden zu optimieren. Nach nur wenigen Tagen erhalten Sie ihr Ergebnis in einem ausführlichen Ergebnisbericht.
Mit Hilfe unseres Testosteron-Testkits entnehmen sich sich eine kleine Menge Speichel aus
dem Mund. Testosteron ist das wichtigste männliche Geschlechtshormon (Androgen).
Es wird beim Mann in den Leydig-Zellen der Hoden und bei der Frau in den Theka-Zellen der
Eierstöcke produziert.
Auf diese Weise kannst Du einen Testosteronmangel oder -überschuss
erkennen und gezielt mit entsprechenden Maßnahmen, wie z.B.
Kosten – Testosterontests zu Hause sind in der Regel viel billiger als Tests,
die in einer Arztpraxis oder einem Labor durchgeführt
werden. So können Sie Geld sparen, wenn Sie Ihren Testosteronspiegel regelmäßig testen lassen müssen. Ein Testosteron Test ist ein Blut-
oder Speicheltest, mit dem die Menge an Testosteron in Ihrem Körper gemessen wird.
ELISA ist eine vielseitige Methode, die wir für
viele verschiedene Tests einsetzen, z.B. Wenn Sie sich additionally schlapp und müde fühlen, ohne ersichtlichen Grund Gewicht zunehmen oder sogar Haare verlieren, steckt womöglich ein gestörter Hormonspiegel dahinter.
Wenn Sie Ihren Testosteronspiegel messen lassen, können Sie später gegensteuern, um Ihre Werte gezielt zu verbessern. Der
Speicheltest richtet sich an Männer und Frauen, die mehr über ihren Hormonstatus wissen möchten. Stress,
Schlafstörungen oder ein unregelmäßiger Menstruationszyklus, können Hinweise auf ein hormonelles Ungleichgewicht
geben. Zusammenfassend lässt sich sagen, dass Testosteron sowohl für Männer als auch für Frauen ein wichtiges Hormon ist.
Es kann auch zunächst ein positiver Check vorliegen, der dann einige
Tage später wieder negativ ist. In einem solchen Fall hat sich der Embryo nicht richtig eingenistet
und wird mit der nächsten Monatsblutung wieder abgestoßen. Das Schwangerschaftshormon hCG (humanes
Choriongonadotropin) spielt vor allem in der Frühschwangerschaft eine wichtige Rolle und trägt zum Erhalt der Schwangerschaft bei.
So fördert es unter anderem die Produktion von Progesteron aus
dem Gelbkörper und sorgt für eine gut aufgebaute Gebärmutterschleimhaut.
Bei der Abgabe eines solchen Tests in der Apotheke sollte die Kundin darüber informiert werden, dass mit der Messung rechtzeitig während des
Menstruationszyklus begonnen werden muss. Beträgt der
Menstruationszyklus beispielsweise 28 Tage, sollte ab dem 11.
Mit diesem Test erfahren Sie, ob Ihr Testosteronwert im Normbereich liegt und ob mögliche Ungleichgewichte bestehen. Hypogonadismus kann
viele Auswirkungen haben, vom Nachlassen der sexuellen Lust (Libido) über Antriebslosigkeit (Drive) bis hin zur Freudlosigkeit (Depression).
Wir helfen Männern in dieser Part wieder zurück auf die Beine.
BEGLEITETE THERAPIE DURCH FACHÄRZTESollten die evidenzbasierten Parameter eine Therapie empfehlen, findet das
nächste Gespräch per Videocall mit Ihrem zugewiesenen Facharzt statt.
Dieser bleibt während der gesamten Therapie Ihr fester Ansprechpartner und steht Ihnen über Ihren Account
in unserem Portal jederzeit zur Verfügung.
Sollten die evidenzbasierten Parameter eine Therapie empfehlen, findet das nächste Gespräch
per Videocall mit Ihrem zugewiesenen Facharzt statt.
Sollten die evidenzbasierten Parameter eine Therapie empfehlen, findet das nächste Gespräch per
Videocall mit dem zugewiesenen Facharzt statt.
Nach der Auswertung des Tests setzen wir uns mit Ihnen in Verbindung, um die Ergebnisse
ausführlich zu besprechen. Diagnose eines Testosteronmangels erfolgt durch eine
Kombination aus der Bewertung der Symptome und
Bluttests, die den Testosteronspiegel messen. Zur Testosteronspiegel-Analyse können auch die von coZERT
empfohlenen Selbsttests verwendet werden. Es ist wichtig, dass die Exams morgens durchgeführt werden, da der
Testosteronspiegel im Laufe des Tages natürlichen Schwankungen unterliegt.
Doch Testosteron ist mehr als ein chemisches Destillat der Männlichkeit.
Testosteron spielt unter anderem eine Rolle beim körperlichen Wachstum, beim Aufbau von Muskelmasse ( anabole Wirkung)
sowie bei der Bildung von roten Blutkörperchen. Zudem ist Testosteron das wichtigste Sexualhormon (Androgen)
für Männer und verantwortlich für die Ausbildung von primären und sekundären Geschlechtsmerkmalen.
Dazu gehören die Entwicklung von Penis und Hoden, sowie eine tiefe Stimme, Körperbehaarung und ein starker Muskelaufbau.
Testosteron ist auch bei Frauen in geringen Konzentrationen vorhanden und beeinflusst den Knochenstoffwechsel,
die Follikelentwicklung, sowie Muskelaufbau und Sexualfunktion.
Es trägt auch zum Sexualtrieb (Libido) bei und spielt eine
Rolle für die Stimmung und das Energieniveau. Bei Frauen spielt
choleriker testosteron – horizonsmaroc.com –
eine Rolle für die Knochendichte, die Muskelmasse und den Sexualtrieb.
Es beeinflusst auch die Stimmung und das allgemeine Wohlbefinden.
bcstaffing.co · May 18, 2025 at 1:03 am
Regardless of why you’re having a blood check, it’s important to keep in mind that while blood checks assist providers
diagnose well being issues, they aren’t diagnoses. If your healthcare supplier
recommends blood exams, they’ll be glad to elucidate why they
advocate the take a look at and what the take a look at
might show. In a wholesome individual, lab exams
are typically inside a sure range considered to
be normal or wholesome. Nonetheless, sure ailments or situations can cause these lab values to deviate from the
traditional vary.
It’s essential to notice that not like allergy pores and skin exams, allergy blood
exams carry no threat of triggering a extreme allergic reaction. For those with skin conditions or on specific medicines that intervene with
pores and skin testing, an IgE blood test could be the safer different.
Pulse oximetry checks are an estimation of blood oxygen levels, but they’re sometimes exact.
This is especially true when using prime quality tools present in most medical workplaces or hospital
settings. With this gear, medical professionals
can perform the tests accurately.
If the distinction is persistently larger than 10 points
between the two arms, let your physician know. This could be an indication that
you have more than anticipated arterial plaque
buildup. The take a look at checks if you have an extreme quantity of or too little of the
hormone. High ranges of certain antibodies might imply
you may have or are at risk steroids for sale online
in usa (bcstaffing.co) sort 1 diabetes.
With years of experience in healthcare journalism, he is devoted to offering clear,
research-backed insights on medical developments and wellness tendencies.
Edgar’s work aims to empower readers with reliable data to make knowledgeable well being decisions.
It’s necessary to keep in thoughts that no check is ideal, and there is
at all times an opportunity of false positive or false adverse
outcomes. This is why follow-up testing or additional
analysis could additionally be needed in certain circumstances, significantly if there are clinical signs or signs that suggest a
sure disease or situation. There are 10 major
things you need to remember to consider on a blood smear.
It Is important to notice that these methods must be mentioned with a healthcare supplier to determine essentially the most acceptable approach primarily based on individual well being wants.
As males age, testosterone ranges usually decline, however this pure decrease just isn’t considered hypogonadism.
The FDA currently advises in opposition to treating
age-related low testosterone in males.
Medical Doctors could suggest a lipid panel for people with risk factors such as smoking, obesity, hypertension,
or a family history of coronary heart disease. The Basic Metabolic Panel
(BMP) & Comprehensive Metabolic Panel (CMP) assess your metabolism, kidney perform,
and electrolyte ranges. Understanding your blood
take a look at outcomes is important for monitoring your well being and detecting potential points early.
However, advanced medical terms and numerical values can make interpretation challenging.
In summary, lab exams are important for understanding
and maintaining your well being. They present useful info that may assist healthcare professionals diagnose
ailments, monitor your health standing, and manage certain circumstances.
By present process lab testing, you can take proactive steps in the direction of maintaining optimum well being and preventing potential well being complications.
If your lab outcomes fall outdoors the normal vary, it might point out that there’s an underlying well being condition that must
be addressed. Irregular lab values can be an early indication of an issue, permitting healthcare providers to take needed actions to prevent additional issues or
to offer applicable treatment. Each lab test has its personal set of ranges which are considered normal or healthy.
These ranges are determined by analyzing samples taken from a large inhabitants of wholesome individuals.
Elevated triglycerides, also referred to as hypertriglyceridemia, can be because of consuming extra calories than you
burn. A high focus of triglycerides will increase your threat for well being situations corresponding to weight
problems, continual renal disease, liver issues, sort 2 diabetes, and pancreatitis.
High-density lipoprotein, or HDL, is dubbed the “good cholesterol” because it removes
unhealthy cholesterol that sticks to the blood vessel wall.
The more HDL there is than LDL, the decrease your threat of coronary heart disease.
Irregularities are a attainable indication of dehydration, adrenal gland disorders, corticosteroids, and kidney or liver issues.
A low platelet volume could cause irregularities
with bleeding, while a high platelet volume can improve an individual’s danger of coronary heart assault or stroke.
There’s no treatment for rheumatoid arthritis, however remedy may help handle your symptoms.
cvbox.com.ng · May 18, 2025 at 6:58 pm
Nonetheless, because of some likely water retention from the
addition of testosterone, it’s extra suitable for bulking.
Winstrol helps you keep muscular tissues
while slicing, and has an insane profit to total athletic performance.
If you’re a woman on the lookout for a steroid and desire a lower probability of virilization (compared to other steroids), then Winstrol might be an option. Winstrol is extra favorable
for chopping muscular tissues rather than bulking. Whereas it could work, it’s not as efficient as other steroids.
Although it’s unlawful in sports activities, Winstrol is a largely
protected, delicate anabolic steroid utilized by men and women alike.
Over time, it has proven to enhance efficiency and physique,
enhance endurance and promote energy without the extra mass.
We haven’t found Deca Durabolin to trigger gynecomastia in most users.
Nonetheless, anecdotally, we now have seen SERMs such as Nolvadex exacerbate progesterone ranges on Deca Durabolin. Subsequently, an aromatase inhibitor (AI) could
additionally be taken, such as anastrozole, to lower progesterone.
However, AIs can worsen blood pressure ranges, so our patients solely take them if the nipples begin to turn out to be swollen. This before-and-after transformation is typical of a bodybuilder’s outcomes
after taking a low-dose testosterone cycle for the primary time.
Winstrol stacks with steroids are decided
primarily by the tip objectives of the users, but Check and Winstrol seem the
best and in style. In an attempt to normalize blood stress, users are
really helpful to take 4 grams of fish oil per day, mixed with wholesome consuming and regular
cardiovascular train. Though endurance activities is
in all probability not what some bodybuilders need to do
when bulking, they can offer cardiac protection. Anavar will worsen testosterone suppression post-cycle,
requiring a more superior PCT compared to a testosterone-only cycle.
Nonetheless, our testing exhibits that Anavar’s antagonistic effects
on endogenous testosterone are gentle compared to different anabolic steroids.
Anavar is usually viewed as a cutting steroid due to its powerful fat-burning results.
This is due to Anavar’s capacity to increase the ratio
of triiodothyronine (T3) to thyroxine (T4) in the physique
(5), stimulating metabolism and fats loss.
In addition to muscle mass, this cycle additionally provides a substantial enhance in strength.
Check Cyp is known for its capacity to enhance pink blood cell manufacturing, enhancing oxygen supply to the muscles.
This elevated oxygenation interprets to improved endurance, stamina, and total
strength. Winstrol, in the meantime, acts as a fat-burning agent, reducing water retention and selling a
leaner physique, further enhancing energy positive aspects.
One of the key advantages of a Test Cyp and Winstrol cycle is the significant enhance in muscle mass.
Your fitness coach may even include a weightlifting coaching program that is best place To buy steroids 2015 (cvbox.com.ng) for beginners.
Throughout these six weeks, users will experience notable muscle growth and
fats loss. Moreover, this mixture additionally aids
in reducing physique fat levels, offering a leaner and more defined physique.
Trenbolone, like Deca Durabolin, presents average progesterone activity,
having the potential to trigger gynecomastia. Thus, users
could wish to avoid using SERMs to prevent aggravating progesterone
levels. Deca Durabolin just isn’t as powerful
as testosterone, so will increase in muscle hypertrophy are unlikely to be excessive.
Nonetheless, as a end result of Deca Durabolin’s mild toxicity,
it may be a complementary stacking element. Thus, if testosterone is the least toxic
steroid, the combination of testosterone and Deca Durabolin may be the least toxic steroid cycle.
Human chorionic gonadotropin (hCG) and Clomid are often adequate
to recover endogenous testosterone production, often within 1–2 months.
Failing to manage PCT may result in users
experiencing low testosterone symptoms for a quantity of months.
Thus, only skilled steroid customers typically
stack Anadrol with other anabolic steroids. Due to the quantity of water retention and bloating they
cause, many anabolic steroids are estrogenic and are referred to as “wet” compounds.
Testosterone and winstrol combo provides the alternative end result.
Thus, a bigger, leaner and extra engaging body might be
achieved with out the dreaded water weight. When you start utilizing winstrol, it’s advisable to take low doses.
This is based on experiences and feedback from
skilled users who attest to its effectiveness even when taking smaller amounts.
For these beginning the Winstrol cycle, it is recommended to take eight mg per day for
the primary 2 weeks.
Anavar doesn’t aromatize or elevate progesterone levels.
Thus, customers might not experience any additional water retention or gynecomastia compared to a testosterone-only cycle.
Hair loss on the scalp, enlarged prostate,
and acne vulgaris are widespread unwanted side effects we see with testosterone and trenbolone
stacks.
The most typical, yet simple and effective cycle of Check and Gainstrol is
the one that’s easiest to make use of. Oral Winstrol
tablets are preferred over long-based Testosterone Cypionate or Testosterone Enanthate.
This stack will produce even harsher unwanted aspect effects
than the Anadrol and testosterone cycle, albeit
with enhanced muscle features. We typically see
Anavar shift levels of cholesterol, decreasing
HDL and rising LDL; due to this fact, a modest increase in blood strain could be anticipated (7).
Testosterone and trenbolone will produce related size gains because the testosterone and
Dianabol cycle but without extra water retention.
This is why we prefer our patients to make the most of SERMs, which block estrogen activity instantly in the breast tissue itself.
Nevertheless, water retention should happen with a SERM as estrogen ranges stay circulating throughout the body.
The above cycle can be seen as a bulking or chopping one, as significant amounts of muscle might be gained together with notable fat loss.
Most generally feel slightly weak 3-5 days after taking steroids.
www.arztsucheonline.de · May 19, 2025 at 11:42 am
Reductions in TC, LDL-C, TG, HDL-C have been observed after one yr of GAHT in contrast with baseline in a
potential cohort research of fifty three transgender ladies [17].
A similar sample compared to baseline was seen in one other cohort
research of 242 transgender women after one 12 months of GAHT [18].
The incidence of cerebrovascular illness in transgender women receiving GAHT was discovered
to be just like sex assigned at delivery men [4] and to the overall inhabitants [5]
in two early retrospective observational studies.
In a retrospective cohort examine of 966 transgender ladies receiving GAHT, the
mortality associated to cerebrovascular illness in transgender women was not statistically different from the final population [10].
Roughly 1.5 million adults in the Usa (0.6% of the population in 2016) identify as transgender,
with ninety nine.5% of those individuals youthful than 65 years [1].
Transgender persons are a various group whose gender id differs from the
sex assigned at start [2].
Regular monitoring of cardiovascular well being is essential for individuals receiving testosterone injections.
This includes conducting baseline assessments earlier than starting treatment
and common check-ups all through the course of therapy.
These assessments might embrace blood strain measurements, lipid profile evaluation, and electrocardiograms
(ECGs). By establishing a baseline, healthcare suppliers can monitor any adjustments that may
occur after starting testosterone remedy.
Given the common use of testosterone in gender-reaffirming remedy, the danger of growing OSA in these
patients must be thought-about, and the patients endorsed on this possible adverse response.
Further research is needed to judge the effect of
sex hormone alternative on sleep-disordered breathing at doses used for gender transition. One limitation of the study is
that it solely accounted for whether individuals had
ever used any type of hormone alternative therapy.
Research has been carried out to untie the knot between testosterone and heart disease.
In Accordance to “Testosterone and the Heart” by Goodale et al., testosterone affects many features of coronary heart health.
A deficiency in this energetic hormone ends in poor cardiovascular outcomes.
Let them know if there are any changes when you are on hormone therapy, or should you get any new signs.
If there’s a rise in your PSA stage, this might be a sign that your cancer has come again. Long-term hormone therapy
might cause your bones to gradually lose their bulk. LHRH agonists, GnRH antagonists and surgery
to remove the testicles (orchidectomy) can all have this effect.
This can occur within the first 12 months of starting
therapy and the amount of bone loss might enhance the longer you
may be on remedy. Anti-androgen and oestrogen tablets are less more likely to trigger bone thinning.
In most circumstances, these adjustments final for as lengthy
as you may be on hormone therapy.
So for something that shapes your masculinity – strength, assertiveness,
authoritativeness – testosterone plays a task. One of
the most effective methods to reduce coronary heart illness danger while on TRT
is by making healthy way of life changes. These changes can considerably enhance cardiovascular
well being and overall well-being. Additionally, TRT can worsen sleep apnea, a condition the place respiratory
stops and starts throughout sleep.
Adequately powered randomized clinical trials designed to evaluate cardiovascular occasions are required to definitively determine the effect of
testosterone therapy on cardiovascular danger. Low testosterone ranges can lead
to increased blood pressure, which is a significant threat factor for heart
disease. Testosterone performs a job in regulating vascular function, and when ranges are low, it
might lead to stiffer arteries and higher blood pressure.
There is a few evidence suggesting that TRT may help improve certain cardiovascular danger factors, like decreasing fats mass, improving
insulin sensitivity, and lowering cholesterol.
However, TRT’s general impression on coronary heart disease
threat continues to be debated, and more analysis is needed to attract clear conclusions.
It is unclear if the increase in cardiovascular morbidity and mortality in transgender women is
due to alterations in cardiovascular danger factors or a direct impact of
GAHT. The present literature, nonetheless, has not shown a consistent undesirable alteration in typical cardiovascular threat components (i.e., hypertension, hyperlipidemia,
and diabetes) in transgender ladies receiving GAHT.
Open communication ensures that emotional unwanted facet effects are
addressed early and treatment stays balanced and effective.
Some men report mood swings, irritability, or a brief temper, particularly in the preliminary weeks of remedy.
These shifts are often an indication that the dosage might have adjusting or that the body is still stabilizing.
We’ll stroll through both the common and fewer typical unwanted facet effects of
TRT, what countries are steroids legal (http://www.arztsucheonline.de) to expect, and the method to handle
them safely with proper medical help. One of probably the most persistent myths round TRT
is that it makes males overly aggressive or “unnatural.” The reality?
is there a legal steroid · May 21, 2025 at 9:32 pm
We have already mentioned the LHRH agonists and antagonists
that are used to treat superior prostate cancer.
These prescription drugs decrease testosterone to castrate ranges by shutting down LH manufacturing by the
pituitary gland. SSRIs are fairly effective at treating despair and are sometimes first line
therapy for men affected by temper problems. Nevertheless,
they do cause quite a number of side effects including sexual
dysfunction.
Furthermore, you will want to observe that particular person responses to testosterone dietary supplements
can range. Some individuals could additionally be more delicate to
the effects of testosterone on blood strain, while others might not experience
any changes. It is crucial to seek the assistance of with a healthcare skilled before
starting any testosterone supplementation, particularly if you
have a history of cardiovascular disease or hypertension. In conclusion, while testosterone dietary supplements from GNC can present quite
a few benefits for males’s well being, it is essential to concentrate on the
potential effects on blood strain. Components similar to dosage,
individual variations, existing well being circumstances,
life-style factors, and period of use can contribute to adjustments in blood
strain.
It becomes more probably when a younger adult under
40 develops high blood pressure, or when a patient needs three or more drugs to
realize blood pressure management. Different warning indicators embody unexplained low potassium ranges and a
family history of early-onset hypertension or stroke. What if
your high blood pressure isn’t just genetic or stress-related—but caused by a hidden hormone
imbalance? Hyperaldosteronism is there a legal steroid a lesser-known situation that could be silently driving your numbers up.
In this article, discover how hyperaldosteronism affects the body—and why early detection could make all of the distinction. So, men with hypogonadism may have a higher response to testosterone than men with greater testosterone ranges who take exogenous androgens.
In TTh-untreated men never given antihypertensives, systolic BP increased at every time point being important
after 12 months follow-up (Fig. 2A). The enhance in diastolic BP (Fig.
2B) and pulse strain (Fig. 2C) in these men was important
after forty eight and ninety six months, respectively.
At baseline, the 353 men on TU, 152 men weren’t on antihypertensive remedy whilst the
remaining 201 men have been beneath therapy for hypertension (Fig.
1B). Significant decreases (median [IQR] in BP and pulse strain values have been noticed in each groups (Table 1 footnote).
I imagine it’s these durations of extra testosterone that create unwanted
unwanted facet effects.
It is important to consult with a healthcare professional if you have concerns concerning the potential
effects of lisinopril on testosterone levels or any other unwanted side effects.
They can provide customized recommendation based
on your specific health circumstances and wishes. To date, there have
been no documented instances specifically attributing lisinopril
to decreased testosterone ranges in males. Clinical trials and studies on lisinopril haven’t reported
any vital modifications in testosterone manufacturing or
hormone levels in male patients. Therefore, it can be concluded that lisinopril does not have a direct impression on testosterone ranges.
Symptoms of coronary heart failure, corresponding to shortness of breath, swelling, and fatigue, are necessary to acknowledge if you’re present
process TRT. TRT could enhance the danger of fluid retention, blood strain modifications, and
other components that may exacerbate these signs.
By blocking this enzyme, lisinopril helps to loosen up and widen the blood vessels,
decreasing blood stress. Another research published in the Journal of Clinical Pharmacology in 2015 also investigated the effects of lisinopril on testosterone levels in males with hypertension. The outcomes of this
examine similarly confirmed no significant changes in testosterone ranges after 12 weeks of lisinopril
treatment. While some supplements may supply sure well being
benefits, others can raise blood stress or negatively work together with blood pressure-lowering medications.
Cardiologists and dietitians agree there are specific dietary supplements you shouldn’t
take when you have hypertension, particularly bitter orange, licorice root,
caffeine, yohimbine and ephedra. As A End Result Of supplements can include
multiple components, it’s particularly important to take the time to learn the ingredient record.
For instance, low T can contribute to hypertension, a condition that impacts practically half of all adults within the Usa and is a
significant risk issue for coronary heart illness and stroke.
One Other study published in the Journal of Hypertension seemed at the effects of testosterone alternative remedy on blood strain in older males with
low testosterone levels. The study discovered that testosterone remedy didn’t significantly
increase blood stress in these individuals. Testosterone
therapy is usually used to deal with hypogonadism, a condition by which the
physique does not produce enough testosterone. This therapy has been shown to have
many benefits, together with increased muscle mass, improved bone density,
and elevated libido. Nonetheless, there have been issues raised concerning
the potential for testosterone therapy to extend blood pressure.
To decide if testosterone levels are impacting blood strain, individuals can bear a blood test to measure their testosterone levels.
Aside from high blood pressure, there are a variety of well being points which are linked to ED, similar to diabetes and excessive ldl cholesterol.
To get to the basis of what’s causing your ED, you can take a
blood take a look at, such because the Sexual Performance Check Package.
This will measure important biomarkers similar to cholesterol and testosterone.
These remedies help stimulate the body’s personal production of testosterone
rather than supplying it externally.
Pin-It.Top · May 22, 2025 at 10:12 pm
The Act was amended in 1987 to permit for the decriminalization of marijuana with out regard to the
age of the offender. This modified when state legislation amended by the Oregon decriminalization system made possession of marijuana
authorized for minors for the first time, anabolic steroids street names.
Abusing anabolic steroids can lead to severe long-term or doubtlessly everlasting well
being issues, with some points being gender-specific or age-specific.
While it’s troublesome to know precisely how someone’s
body will react, utilizing steroids always poses
some level of danger.
Dianabol is produced by quite a few manufacturers and goes by many names.
Dbol Reforvit, also called Reforvit-B, is the commerce name of one of the potent and purest types of Dianabol steroid.
If you have a hard time deciding which to choose, here’s a brief outline of each types – hopefully we might
help you choose right. However when HGH melts fat, the sudden dump of
glucose into your bloodstream can overwhelm the conventional processes
that clear it, leading to a danger of insulin resistance and diabetes.
What’s extra, there is not any evidence that HGH will allow you to live longer.
Since HGH promotes the expansion of tissue
all through the body, fledgling tumors that will grow
slowly or by no means may get a jumpstart into malignancy.
Danish researchers are additionally wanting into
HGH as a remedy for patients with tendinopathy—long-term
tendon pain.
“Gym candy” highlights how these medicine are perceived as enhancements for gym-goers, making them sound virtually like a deal with rather than a probably harmful substance.
You’ve realized about numerous anabolic steroids road names, which play a vital function in understanding the underground market.
These names usually sound harmless however mask
the risks and penalties of steroid use. “Roids,” “juice,” “gym candy,” and “Arnolds”
are among the many most typical terms you’ll encounter.
Salvia is a robust psychedelic drug legal in plenty of
parts of the world. It is derived from the salvia divinorum plant and can be consumed by chewing, smoking, or consuming it as
a tea. Rohypnol can even cause amnesia, which means that victims could additionally
be unable to recollect what occurred to them while under the drug’s influence.
As A Outcome Of of those results, Rohypnol is particularly
harmful when used with no person’s consent.
Nonetheless, folks utilizing it recreationally can expertise unhealthy journeys characterised by
nervousness, paranoia, and delusions.
It is an artificial version of human male sexual-hormone aldosterone that has a
better affinity to the human physique than natural aldosterone.
It is derived from the acesulfame-K enzyme, which is the enzyme responsible for converting aldosterone to its lively kind, the lively substance DHT, in the human body.
The time period has also been referred to as anabolic-sex steroid as a result of it’s similar in appearance to a steroid like testosterone, however has less exercise and fewer of the unwanted effects of Steroids Side
Effects – Pin-It.Top – just like the high androgenic side effect.
Schedule I medication are these the DEA has determined to
have a excessive potential for abuse and no accepted medical use.
They embody medical anesthetics (ether, chloroform, halothane, and nitrous oxide) and family and business products (whipped cream
dispensers, butane lighters, propane tanks, and refrigerants).
Methadone, buprenorphine, and naltrexone are all FDA-approved medications to treat
opioid use disorder (OUD).Lofexidine is an FDA-approved medication to reduce opioid withdrawal symptoms.
Dissociative medication can briefly alter
a person’s mood, ideas, and perceptions of actuality.
These medication primarily have an effect on how the
brain processes a chemical known as glutamate.
Some folks use tobacco for its stimulant results, but it can be
addictive and harmful to general health. Tobacco is a plant that accommodates the psychoactive
substance nicotine. Nicotine is a stimulant that can have each positive and unfavorable effects on the brain. In some circumstances, customers have even been known to experience “excited delirium,” a situation marked by hyperthermia, superhuman strength, and agitated hysteria.
Synthetic cathinones, also identified as “bath salts,” are psychoactive drugs that mimic the consequences of cocaine and methamphetamine.
Artificial cannabinoids affect the brain by binding to the same receptors as THC.
This may cause similar results as marijuana, including altered perception, mood,
and conduct.
Throughout head influence or whiplash, your mind can shift inside your cranium.
The pituitary gland isn’t a part of the mind however sits at its base, connected
to it by a tiny stalk. But if his analysis turns out to be successful,
it might usher in a new era of better, quicker recovery from sports activities injuries.
“If you spend as a lot time in the health club world as I do, you pretty properly know how to acquire it,” he says.
Larry’s supply comes from a particular relationship
with a physician. Individuals who can’t get prescription HGH typically discover a dealer who orders it from China.
Apparently, loads of athletes and celebrities are already true believers.
These receptors play a job in zits formation when Propionibacterium acnes micro organism are also current.
Folks who abuse anabolic steroids might have a weakened
immune system. Strong immunity is critical to guard the physique
in opposition to micro organism, viruses, and different invaders.
By weakening the immune system, anabolic steroids put a person at
a better risk of creating varied ailments.
As talked about above, these steroids are also known as anabolic-androgenic steroids where “anabolic” stands for muscle
constructing and androgenic refers to enhanced male
intercourse characteristics. The common age vary amongst anabolic steroid customers is from the mid-20s to
mid-30s. The most frequently used body building steroid has been Dianabol.
zghncy.cn · May 23, 2025 at 12:10 am
70918248
References:
safest oral steroids (zghncy.cn)
click4r.com · May 23, 2025 at 12:43 am
70918248
References:
steroids good (click4r.com)
Iti.Vnu.Edu.Vn · May 29, 2025 at 10:28 pm
If you need to enhance your performance safely, there are significantly
better options out there than this dangerous
drug. If you want to bulk up, you’ll need a higher dosage of mg per day.
The answer to this question will determine the
size and dosage of your cycle. It Is true that Winstrol
has some superb benefits, but it additionally comes with its
justifiable share of unwanted effects. Simply be sure to communicate with
your doctor first and be certain to perceive all of the
dangers concerned.
Thus, we think about it to be the least deleterious selection for
someone’s first cycle, as nicely as performing as a base
compound for experienced bodybuilders stacking a number of compounds collectively.
Dianabol and Anavar stacked collectively may
seem uncommon, as Anavar is a cutting steroid with diuretic results, whereas Dianabol is a bulking steroid that promotes water retention. Dianabol also will
increase visceral fat storage, while Anavar decreases it.
However, we have observed this unconventional stack to be an efficient bulking protocol, as Dianabol
increases muscle mass and Anavar concurrently prevents fat accumulation.
Steroids that don’t increase estrogen ranges are usually less effective for muscle development.
This is why individuals who only take a Winstrol cycle typically don’t make
the dramatic size gains that people taking testosterone,
Dianabol, and different estrogen-producing steroids do.
When it involves gaining muscle or bulking, Winstrol is widely thought-about a
steroid that isn’t appropriate or efficient for males.
However it’s not just testosterone itself that’s liable
for any androgenic unwanted aspect effects you might develop.
Mostly, it’s the conversion of testosterone into DHT (dihydrotestosterone), which is an much more highly effective androgen that’s
the offender of much of the dreaded unwanted effects in this class.
On prime of this, your genetics will largely decide if and
the way severe these side effects could be.
EQ has less estrogenic activity than Dianabol, however all testosterone-derived steroids can result in the
event of water retention. Testosterone derivatives are sometimes favored extra for bulking cycles somewhat than slicing cycles the
place fluid retention is undesirable. After you achieve some experience using a particular steroid, you’ll get a good suggestion of whenever you really feel the benefits reducing.
You’ll then be able to plan your cycles extra
exactly to achieve maximum benefit from each steroid. Lots Of of 1000’s
of individuals have already worked out the perfect method to use
them, so there’s little reason to attempt to reinvent the wheel.
Nolvadex PCT is taken into account a good PCT selection for more mild steroid
cycles. It helps restore your natural hormone
exercise and comes with minimal threat of side effects.
A seriously superior Winstrol cycle adds in Trenbolone – one
of many hardest steroids to use and solely suited to the most skilled
customers. These two potent steroids mixed can create important dangers if you don’t know what you’re doing.
These steroids will provide speedy outcomes that can deliver a few very fast physique transformation in a short
and sharp 6-week cycle. Winstrol is a strong anabolic Growth Steroid –
Iti.Vnu.Edu.Vn, that
can allow you to achieve vital gains in muscle mass and strength.
However, it also comes with a bunch of potential unwanted side effects that can be dangerous to your well being.
I’ve heard of men utilizing it for ten weeks or longer, but this is discouraged, and more so, there are no vital advantages to utilizing Winny for thus lengthy.
If you’re predisposed and sensitive to hair loss and pimples,
note that it could possibly nonetheless occur at a decrease dosage.
Winstrol is unique among the many steroids that exist in each oral and
injectable types in that Stanozolol is C17a alkylated in both codecs.
A frequent strategy on a Winstrol cycle is to make use of
your comfy maximum dosage within the last week or two before a contest
and a decrease dose earlier. Winstrol will promote power gains at a stage that may be shocking, particularly when we consider it
as a slicing steroid. Maintaining energy while weight-reduction plan is crucial, but Winny can significantly improve
strength past primary maintenance.
These are only a few of the things that may go mistaken when injecting steroids.
Most people will expertise a problem a technique or one other when utilizing steroids over many years.
It’s finest to study what minor or main concern wants more instant consideration or care.
The addition of the thyroid hormone Cytomel on this superior cycle assists in regulating metabolism and energy.
These much longer superior cycles that stack a number of steroids
are superior cycles. Females who develop virilization are always
advised to cease use immediately so those effects can subside
and disappear.
Because different factors will influence the half-life of any steroid,
together with your metabolism. Nonetheless, the approximate half-lives which
might be identified for all our generally used anabolic steroids present a solid base to plan your cycles on. The most universal of all steroid effects is a rise in protein synthesis19,
with nearly every steroid selling protein synthesis to a
point.
Anabolic steroids, when utilized by females, result in the event of male
physical options. Girls can use Winstrol at
very low doses with little or no risk of these virilizing side effects, but
at doses of 15mg or more every single day, a female runs a excessive risk
of changing into extra masculine in some ways. Although she won’t flip into a
man, this powerful androgen, when used at excessive doses or for too long, will take away femininity and cause a lady to look
and sound very completely different.
human Growth hormones steroids · May 29, 2025 at 11:57 pm
It boosts the production of hormones like FSH and LH, necessary for both women and men.
In males, it is used for hypogonadism attributable to steroid abuse, helping to steadiness hormones and improve testosterone ranges.
Incorporating recovery dietary supplements like ZMT by Swolverine may help regulate cortisol,
enhance sleep, and help natural testosterone manufacturing by
way of focused micronutrient help. Some bodybuilders go for natural testosterone boosters during their PCT instead of pharmaceutical interventions.
These supplements typically contain elements like Tribulus Terrestris or D-Aspartic Acid,
which claim to reinforce pure testosterone manufacturing.
By implementing an effective PCT routine, people can restore hormonal
balance, protect muscle positive aspects, and scale back the probability of creating these unwanted effects.
The brands talked about here can be obtained legally both online or over-the-counter.
They can be found in the USA, Canada, the UK, Australia, and many different countries.
With these brands, there’s additionally no need for post-cycle therapy (PCT).
Past its use in bodybuilding, Clomid is typically prescribed to ladies who’re having difficulty ovulating as a fertility drug.
Clomid, identified extra formally as clomiphene citrate, is
an artificial non-steroidal drug that has a structure much
like estrogens. This powerful, all-natural supplement has been formulated to
specifically target chest fat and assist you to burn excess fats with exercise and nutrition plans created by consultants.
Gynectrol is a powerful supplement that helps to reduce the
dimensions of man boobs by focusing on the underlying fats cells.
Post Cycle Remedy (PCT) isn’t nearly recovering from steroid
use; it’s about coping with real challenges.
From erectile dysfunction and muscle loss to mental well being struggles,
the consequences are sometimes greater than expected.
I also discuss the temptation to return to steroids when your physique starts to lose its features.
The minimum timeframe for HGH use is 16 weeks, however 24 weeks
is recommended for greatest results. The stacked steroids
will usually be added to the second half of your cycle.
Relying in your specific goals, these will typically be the most popular steroids,
like testosterone and Trenbolone for bulking cycles and Anavar or Winstrol
if you’re on a chopping cycle. For probably the most hardcore fat loss, Clenbuterol (which just isn’t a steroid)
is usually stacked with HGH. Deca Durabolin and Anadrol are different steroids
that males will stack with HGH. If you’re
taking doses of 8iu or more, splitting it into two
daily injections isn’t unusual.
This guide tells you everything you should know about PCT, such as when to begin, what post-cycle remedy does
what to take for post-cycle therapy, and the best methods to keep the load off after a cycle.
The 2024 Dubai Pro occurred on July 28 in Dubai, United Arab Emirates,
and was arguably the biggest competition on the bodybuilding calendar.
With the record of participants that was fashioned and the grand prize of $100,
000 for the winner of the Males’s Open Bodybuilding class,
the competition was expected. There aren’t any such disadvantages reported about
PCT medication; however, for a number of hypersensitive customers,
it may cause unfavourable penalties. If you are consuming it for
improved bone therapeutic and bone mineral density,
then 50 to 100 mg per day is the advisable dosage.
Whereas, if one is taking it for erectile dysfunction, vaginal dryness,
or menopause signs, then 25 mg to 50 mg per day is a adequate shot.
In the past few years, HCG has turn into popular in the bodybuilding and sports industries for numerous profitable causes.
Anabolic androgenic steroids are synthetic derivatives of testosterone, which
is the first male intercourse hormone. Anabolic androgenic steroids are
used to enhance athletic performance and appearance.
Antagonistic effects include those on the liver, serum lipids, psyche/behavior and reproductive system.
From boosting hormone production to supporting
testicular operate – this potent hormone, often known as hcg, wears many
hats. Alongside its role in boosting testosterone ranges,
chorionic gonadotropin, also recognized as hcg publish cycle,
helps sperm manufacturing – one other important facet of
restoring hormonal well being during PCT. Dianabol is not FDA-approved and thus isn’t considered safe for human Growth hormones steroids consumption. There are dangers when taking Dianabol and different anabolic steroids,
particularly to the heart, liver, and testes. SERMs work by
blocking estrogen levels immediately in the breast tissue (6), versus
inhibiting the conversion of testosterone into estrogen. This way, estrogen ranges do
not lower, stabilizing cholesterol whereas considerably decreasing
the risk of gynecomastia. Tamoxifen (Nolvadex) and clomiphene (Clomid) are the two
main drugs we use to forestall Dianabol-induced gynecomastia.
Don’t leave your restoration to likelihood; choose our PCT for optimum
post-cycle outcomes and guarantee your hard-earned features stick with you.
This article will current forth the very best and best post cycle remedy protocol backed by valid scientific data and logical reasoning.
Now you understand what you have to do and the way you should do it,
however you proceed to don’t have the proper doses or full time frame on your submit cycle remedy remedy and that’s the ultimate level of our discussion.
Our results also indicated that CRP levels 2 weeks after VDZ induction can affect the continuation fee within the VDZ + rPSL group.
CRP ranges 2 weeks after VDZ induction could affect the continuation fee in the VDZ + rPSL group.
Underground lab HGH comes with many risks, not the least of which is the under-dosing of the formula.
The arms and ft, in addition to the jaw area, can become noticeably
larger. All of this will result in serious health impacts and
stress brought on to very important organs. Liver harm
also can become a long-term opposed impact after
sustained HGH use.
steroids vs testosterone boosters · June 1, 2025 at 5:30 pm
Testosterone additionally has Trenbolone-like qualities together with increased power
output so you can lift heavier weights to induce more hypertrophy.
This is the most plentiful male intercourse hormone produced by our our bodies naturally.
Utilizing Trenbolone along with testosterone can result in wonderful muscle features which are hard to match.
Trenbolone is an injectable steroid, whereas
testosterone is a pure hormone.
Males who’re utilizing Tren must take Testosterone to complement the amount that’s the physique is
producing. In addition, Trenbolone is a Progestin, a hormone that’s responsible for
the menstrual cycle. It can set off the manufacturing of Prolactin, a protein that allows
mammals to produce milk. This situation can forestall the kidney from eradicating water from the
bloodstream, leading to the rise of the blood pressure.
Others might react negatively to a single dose
while others may not feel anything regardless
of utilizing the steroid for a long time. Having big and pronounced muscles and veins are
one of the indicators of being physically match.
Since it’s robust, introducing this compound to the system leads to a
response. You can count on unwanted effects
with a higher dose of Tren, which is greater than 400 mg per week.
So, contemplate this dosage only if you have tolerated or handed the intermediate cycle.
Since it’s a potent steroid, getting medical recommendation before
you undergo the Tren cycle is advisable. You ought to
adhere to strict supervision adopted by effective PCT (Post Cycle Therapy).
It is initially meant for veterinary use to extend the physique mass of the cattle.
Since tren offers each bulking and chopping advantages, it’s
a versatile choice for people with totally different fitness
goals. Nevertheless, accountable cycling is crucial to stop
potential well being dangers. Trenbolone pills are a safer different to conventional injections,
offering customers a handy and legal choice for incorporating this potent steroid into their health regimens.
These pills mimic the consequences of trenbolone, selling muscle progress and enhancing total efficiency.
It permits you to evaluate your response unique
to this steroid before you consider stacking it with any others.
This places you above commonplace testosterone substitute, but not an excessive dose that causes extra prominent side effects.
Another aspect of your outcomes with this steroid will relate to
restoration. You should discover less time to recuperate from intense exercises and less muscle pain post-workout.
Not solely will heavier lifting functionality contribute to your outcomes with Testosterone Cypionate, however so will the elevated
endurance and stamina you feel.
Between these quick cycles, you can use Clomid or Nolvadex if you’re nervous about LH and FSH levels, however more typically than not,
they rebound properly. This means such a brief cycle will be favored
by individuals with particular causes to run a cycle of this length rather than a normal
one. You could use nearly any quick injectable
ester or oral steroid as a secondary compound in a 6 to 8-week cycle.
The typical selections are Anadrol, Winstrol, Trenbolone Acetate, Masteron Prop, Dianabol, and
Anavar. Proviron is another compound worthy of consideration for the standard chopping
cycle. It’s also a DHT-derived oral steroid, however it’s thought-about one of many extra milder
compounds. Primobolan can be a DHT-derived steroid, and it’s an excellent one
to make use of in lengthy cycles as it’s a tolerable compound with decreased
androgenic results and milder testosterone suppression.
What is that you would be be asking, nicely, she or he simply realized to cease saying that stereotypical stuff that so many
do, that’s, “he or she looks like that simply because of the steroids”.
In veterinary medicine, trenbolone was initially developed to promote muscle progress in livestock.
Today, it stays one of the most powerful anabolic steroids out there, valued for its effectiveness in both bulking and chopping cycles.
For greatest results, users should run trenbolone with a well-structured cycle, taking into account the synergy between testosterone and trenbolone.
Biking Check and Tren collectively is well-liked
amongst bodybuilders and athletes because the mix can significantly improve muscle mass and power gains.
Testosterone supplies a stable basis for total muscle growth and restoration, whereas Trenbolone is thought for its capacity to promote lean muscle development and fat loss.
In truth, it’s one of the primary the reason why individuals typically use trenbolone
– to reduce back the unwanted side effects of low testosterone levels.
We all know that, but I needed to reiterate it for everybody on the market.
Once I cycled with Tren Enanthate my experience with the
side effects was not almost as bad as after I
used the Acetate version. I am the kind of guy who likes to strive everything a
minimum of as quickly as in my life, steroids vs testosterone boosters aren’t any exception.
My calorie consumption was bumped up fairly a bit and my workouts grew to
become more intense. The use of Tren Enanthate in my bulking cycle allowed my body to maintain pushing via the exercises
better than I would without it.
best anabolic steroid for weight loss · June 4, 2025 at 3:26 pm
Composed of short chains of amino acids, peptides are signaling molecules that regulate numerous processes from metabolism to tissue
development. Synthetic versions claim to crank up fat burning, enhance sleep quality, or accelerate restoration. That’s “selective androgen receptor modulators,” and within the
Nineteen Nineties they had been considered as a safer various to steroids.
Most commonly taken orally, SARMs remain in style (boxer Ryan Garcia failed a drug take a look at for them recently) and are similar
to steroids in that they target androgen receptors.
Thus, although a major quantity of the steroid will
be energetic because of C17-alpha alkylation, if you’re taking 30 mg of Dianabol,
the true dose may only be 26 mg. In contrast, users who inject 30
mg of Dianabol will experience the full dose.
Injectable Dianabol is an possibility for people who don’t want to experience liver issues when taking
this steroid. Dianabol is often an oral steroid; nonetheless,
there are veterinary variations of it out there that might be injected, immediately coming into your bloodstream and bypassing
the liver. However, we discover injectable Dianabol to be less widespread on the black market, with orals
being the more commonplace form of administration. The liver is a resilient organ with
robust self-healing properties (commonly regenerating itself post-cycle).
If there might be one thing Loopy Bulk may do to enhance, it would be to decrease
their prices even additional and enhance their average review
rating from four.4/5 to 5/5. If you’re critical about doing it right, shield your physique, run your labs,
and let outcomes and recovery drive your decision-making — not ego.
Many users select to run one or both SERMs depending on their cycle size and compound intensity.
Doses beyond this range significantly enhance danger without guaranteeing higher results.
But like all synthetic supplement, they are often dangerous and even lethal
when misused, whether or not you utilize too much or for
too lengthy a time. While it can be difficult to avoid falling for PED marketing techniques
and influences, Hemendinger says there are a few steps to take
to apply physique acceptance and neutrality. First step,
balancing your social media use and realizing when these feeds aren’t serving you.
This is the optimal protocol rather than taking drugs corresponding to diazepam, as they put further strain on the liver (28).
Even natural sedative supplements, such as valerian root, are able to having an adverse effect on liver values.
We have discovered that anabolic steroids, together with Anadrol, could
cause insomnia in some customers because of extreme CNS stimulation. We discover the
lean muscle features skilled on Anadrol are often everlasting.
Just over half of the burden a person gains from Anadrol might be lean muscle (the rest might be water).
Another reason why Anadrol is female-friendly is as a result of of its low affinity when binding to SHBG (19).
These compounds are designed to mimic the results of naturally occurring testosterone,
enhancing muscle growth (anabolic effects) and promoting
male physical traits (androgenic effects). As precisely reflected by
their anabolic and androgenic scores, Dianabol is the superior steroid for building mass.
Nevertheless, Deca Durabolin is an efficient compound that
can maximize muscle and energy features when mixed with Dianabol (or
other mass-building steroids). Several medicine can be taken following Dianabol cycles to help restore natural testosterone manufacturing.
The following is an aggressive PCT protocol designed by Dr.
Michael Scally, a leading expert in hormone replacement.
This was used in a medical setting on 19 males, by which one
hundred pc of them recovered their pure testosterone production 45 days after taking steroids.
Furthermore, some research suggests DHT could be the
better muscle-building hormone when in comparison with testosterone (23).
Anabolic steroids have many dangers, making it necessary to know what they’re.
The safety and effectiveness of every product depends on the manufacturer.
We have done in-depth analysis to find essentially the most reputable corporations that present all-round safe merchandise that provide a number of benefits with
no dangerous side effects. We assessed the general worth of every legal steroid,
taking into account its safety, formulation transparency,
manufacturer’s credibility, and value. We evaluated the value of each legal steroid to ensure it offers good value for cash.
We favored supplements which would possibly be moderately priced with
out compromising on safety.
What makes D-Bal even more appealing is that it’s made with high-quality and safe components.
Healthy fat and omega-3 fatty acids are simply as essential for a balanced food regimen that fuels muscle strength.
They help scale back inflammation and support cell health, which improves restoration after workouts.
Reveals that consuming plenty of healthy fats boosts the physical form and performance of energy athletes.
It’s key for those seeking to increase muscle growth and energy to observe the right vitamin plan. Consuming a balanced food regimen filled with essential vitamins
helps enhance your physical talents and recovery time.
Traditionally, safed musli has been used to spice up efficiency,
by enhancing stamina and muscle energy.
One complement that is well-liked with athletes known as creatine monohydrate.
It Is common for athletes who exercise for long quantities of time to make use of a lab-made sort of
erythropoietin known as epoetin. This is opposite to different oral steroids,
that are C-17 alpha-alkylated and must be consumed on an empty abdomen for full results.
This is as a end result of of most orals being fat-soluble and thus susceptible to
decreased absorption through the gastrointestinal
tract.
DecaDuro is among the top-rated legal steroids as
a outcome of it encourages muscle development naturally and boosts the physique’s ongoing manufacturing of
progress hormone. The complement is good for anybody above the age of 18 who goals to extend their lean muscle mass
and forestall the buildup of extra fats whereas sustaining their endurance ranges.
Individuals in search of alternatives to conventional steroids often turn to natural dietary
supplements. These choices may help build muscle with out
the risks linked to best anabolic steroid for weight loss steroids.
Common choices embrace products that use elements like creatine, protein powders,
and branched-chain amino acids (BCAAs).
how do steroids work in the body · June 5, 2025 at 3:45 am
An various to those illegal steroids is natural dietary supplements (testosterone boosters) that work pretty much as good, however they’re safer and
better than their artificial counterparts.
Legal steroids are a subcategory of bodybuilding dietary supplements
designed to mimic the muscle-building effects of anabolic steroids—without the side effects or authorized issues.
Unlike banned substances like Dianabol or Trenbolone,
authorized steroid options are created from natural, safe
elements and are totally legal to purchase
and use within the USA and a lot of different international locations.
People on the lookout for alternatives to conventional steroids usually turn to natural supplements.
These options may help construct muscle with out the dangers linked to anabolic steroids.
Common selections embody products that use ingredients like creatine,
protein powders, and branched-chain amino acids (BCAAs).
While anabolic steroids would possibly appear to be a tempting shortcut, their potential unwanted effects, including liver harm, hormonal
imbalances, and cardiovascular issues, make them a dangerous alternative.
Luckily, there are pure alternate options to how do steroids work in the body like Prednisone that may, indeed, assist
relieve irritation. Long distance operating could
provide an efficient cardiovascular workout, yet can actually have a unfavorable effect on testosterone ranges when combined with
vigorous training and health levels. Whereas the bent over
row might help increase testosterone levels, proper type and approach have to be observed to avoid injury and target particular muscle tissue successfully.
Research have demonstrated that compound workouts similar to squats and bench presses
enhance testosterone levels extra successfully than isolated
workouts. Estrogens are steroid hormones that play an essential function in each
male and female reproductive capabilities, together with cognitive health,
bone well being and cardiovascular system efficiency.
To construct muscle, testosterone should interact with muscles and bind to receptors referred to
as androgen receptors in cells.
For occasion, the side effects and their depth
by taking oral steroids are different from those of intravenous steroids.
However, turmeric is way extra superior to steroids due to its low toxicity
and low costs. Steroidal, medication have a high fee of occurrence of unwanted facet effects some of those being
non-reversible.
Most individuals are able to see results within two to three months, however when the dietary supplements are used along with a healthy diet and exercise, the results can present up
inside weeks. Such people ought to never lose hope and be in preserving with the
usage of dietary supplements. Legal steroids are dietary dietary supplements
that can be bought domestically or on-line.
You don’t need post-cycle therapy (PCT) after taking turkesterone as a result of it
doesn’t influence your testosterone ranges. Subsequently, suppression doesn’t happen after utilizing the complement,
which ultimately eliminates unwanted side effects and improves retention of muscle positive aspects.
It’s simply the right addition to an already-effective lifting cut up and food plan to assist you gain extra lean muscle mass and increase strength.
Ecdysteroids can enhance the adenosine-5-triphosphate (ATP) content material found in muscle tissue.
Primarily, the more ATP synthesis, the better you can perform endurance and energy exercises.
If you are presently taking prescription drugs, contact your
doctor before utilizing this product. The general consumer score is basically favorable,
with many people claiming important muscular growth. When you purchase a six-month
quantity, the price drops to $46.sixty four every month.
For those looking for an extra boost to beat efficiency plateaus or slumps, it’s really helpful
to seek the advice of with a professional, ideally your
private trainer or doctor. Seek The Assistance Of a healthcare professional or a knowledgeable coach who
understands peptide utilization. Due to poor bioavailability
when taken orally, the topical software is way
more practical and will offer localized advantages.
Ask questions about their products, sourcing, and testing procedures to gauge their reliability.
In one study in 210 people with hypertension, garlic tablets had
been even more effective than the blood-pressure-lowering drug atenolol
(34). In people with elevated levels, garlic can decrease
systolic blood pressure (the high quantity in a reading) by 8.32±1.ninety three mm Hg and diastolic blood strain (the decrease number) by 5.48±1.92 mm Hg, on average (33).
They inhibit the production of ldl cholesterol in your liver, leading to
considerably lowered blood levels of cholesterol.
It’s a powerful antioxidant, can improve coronary
heart health, and should assist forestall cancer (15, sixteen, 17).
For example, in a study in 45 folks with rheumatoid arthritis, 500 mg of curcumin per day was more
effective than the anti-inflammatory drug diclofenac (14).
This highlights the necessity for complete research and regulation to make sure
the accountable use of those compounds in the athletic
community. Sure herbs, corresponding to nettle leaf or noticed palmetto, are believed to include
phytosterols and may be brewed into a soothing cup of tea.
This can be a relaxing and pleasant way to introduce plant-based steroids into your day by day routine.
bamchrc.co.in · June 5, 2025 at 12:25 pm
Dangers of Utilizing Unlawful Anabolic SteroidsAnabolic-androgenic steroids (AAS) are synthetic substances derived from testosterone.
Though sometimes prescribed for medical circumstances, they’re usually misused—particularly by athletes and bodybuilders—at dangerously high doses, typically
10 to one hundred instances the therapeutic stage. Some users additionally combine multiple steroids, growing health dangers significantly.
Growing numbers of dietary supplements with ecdysteroids are
marketed as “natural anabolic agents”. Results of latest studies advised that their anabolic impact is mediated
by estrogen receptor (ER) binding.
The closest authorized factor to steroids are sometimes called
legal steroids or the best steroid alternatives. These are supplements
created from pure ingredients that aim to provide a few of the advantages of steroids, like muscle development and efficiency enhancement, but without the same risks and legal points.
Brutal Force’s HBULK is our prime decide among the greatest legal
steroids on our listing, offering fitness lovers a legal various to traditional anabolic steroids.
With a blend of natural ingredients, it aims to assist muscle progress, energy enhancement, and total performance.
To maximize advantages, corticosteroids are prescribed within the lowest attainable dose over the shortest period of time to realize the greatest possible end result.
When unhealthy unwanted aspect effects kick in, the hunt for a perfect physique
becomes much more harmful. They cut back muscle soreness and fatigue, enabling individuals to recuperate extra shortly after
strenuous workouts. Whether Or Not you’re chopping, bulking, or trying
to boost performance, CrazyBulk offers a
pure and dependable resolution for reaching your health goals—safely and legally.
Tren-Max not solely helps to construct lean muscle however to shed cussed fats, which makes it
a great different to D-Bal for the one who is working exhausting however not quite where they need to
be weight-wise. In Accordance to Endocrine Society 2010
pointers, testosterone levels must be measured midway between injections of testosterone enanthate or cypionate.
In addition to their muscle-building properties, these foods may help sustain energy levels during
exercises. A balanced intake of proteins, wholesome fat, and carbohydrates
from natural steroid meals can improve endurance, power, and recovery, resulting
in enhanced athletic efficiency overall. Incorporating these meals right into
a well-structured food regimen can considerably contribute to health objectives.
In conclusion, it’s potential to explore nature’s bounty to discover food that acts as a natural steroid.
By including foods similar to eggs, lean meats, fish, avocados, spinach, nuts,
and whole grains in your food regimen, you’ll have the
ability to promote wholesome hormone production and improve muscle
growth naturally. Anabolic steroids (also referred
to as anabolic androgenic steroids) are synthetic (man-made) versions of the hormone testosterone and associated substances that are typically used to increase muscle
dimension and power. Beans include pure anabolic steroids referred to
as saponins which are recognized to stimulate testosterone
production and decrease cortisol levels, each key elements of muscle
progress.
What really units D-Bal Max aside is its capacity to deliver fast, noticeable results.
Right Here are 5 of one of the best legal steroids for
sale (bamchrc.co.in) legal steroids that have a stable popularity
in the health business. All dietary supplements and types mentioned have a manufacturers assure and are made beneath
Good manufacturing practices (GMP). It’s true that utilizing sure steroids in small amounts
under medical supervision won’t damage you.
However, the characteristics of the three groups have been generally comparable with respect to important demographic parameters.
Additionally, participants were recruited from the
identical communities, which were primarily located
in the greater Copenhagen area. The individuals volunteered from the group and weren’t patients from our clinic,
but we can not exclude the likelihood that this study could have been affected by choice bias.
Recall bias can also have affected our results, as
appreciable quantities of information have been obtained via self-reported histories.
In this research all former AAS abusers exhibited plasma SHBG inside
the regular reference range and excludes that oral AAS have been abused in this group while injections with testosterone
might probably still have been used.
It’s not steroids, but that is certainly probably the greatest steroid alternatives.
ABulk specifically is certainly one of their greatest products because of
the efficiency of the testosterone boosting component particularly.
Almost all the energetic ingredients are clinically
studied natural testosterone boosters, and the most
important ingredient is also standardized to maximum
efficiency. Consider a pure anabolic steroid that comes with a clear
list of elements, so you understand exactly what you’re putting in your body as you’re employed to gain greater muscle.
Selecting a authorized steroid comes all the method down to which brand
delivers essentially the most benefits you’re in search of,
whether it’s a testosterone booster or a post-cycle method.
You can take Rebirth after a cycle to increase testosterone and promote
muscle mass. It also works as a standalone T-booster for lean mass and drive, with 30 servings per bottle.
Used responsibly, Testol one hundred forty
might help you obtain the type of transformation that used to be
possible only with hardcore steroid cycles. Testol one hundred forty isn’t
just another supplement; it’s a legalized SARM that works like RAD one hundred forty, arguably
the strongest SARM in the marketplace. It Is turn out to
be the go-to choice for many bodybuilders who’re looking for steroid-like outcomes without the authorized
dangers or extreme side effects. Testo Prime contains
Ashwagandha extract, which has been proven to extend testosterone levels whereas simultaneously
decreasing cortisol – the stress hormone that can wreak havoc on your positive aspects.
And let’s not neglect about the addition of Fenugreek, which can help free
up certain testosterone, making extra of it obtainable for
use by your body.
Trenbolone is an injectable steroid and helps you achieve massive muscular
tissues with out the extra water weight seen with another steroids like Dianabol.
Dianabol Cycle for Bulking A typical Dianabol cycle normally lasts from four to six weeks.
As A End Result Of it is extremely powerful, it’s often used together with different steroids, similar to Testosterone or Deca-Durabolin, to maximize outcomes whereas keeping unwanted effects low.
If you want to get even higher results, you presumably can mix Dianabol with Trenbolone and Deca Durabolin in a “Bulking Stack.” Nonetheless, with more superior detection strategies,
any steroid testing is undertaken by competitions and authorities with the finances
to make sure in-depth tests will pick up metabolites.
You should not be stunned when these metabolites are still present weeks, months, and generally nicely over a 12 months after you’ve taken your last
anabolic steroid dosage – no matter what that
steroid’s half-life is.
Zarejestruj sie · June 6, 2025 at 2:01 am
Your article helped me a lot, is there any more related content? Thanks!
dianabol Before and After 8 weeks · June 7, 2025 at 2:06 pm
While Dianabol is celebrated for its ability to promote rapid muscle growth
and enhance performance, it also comes with a series of potential side effects.
Understanding these and knowing how to manage them is crucial for any bodybuilder
considering a Dianabol cycle. For increased efficiency, many users opt to
stack Oxandrolone with compounds like testosterone, Dianabol,
and Trenbolone, depending on their fitness goals.
You need to read Straight From the Underground – the ultimate reference guide to steroids.
Your lower back can get these insane cramps or pumps, there were plenty of times I would have to drive home
from the gym with my seat reclined more than normal to deal with the back
pumps. You’ll hear a lot of talk about not using Dbol solo, but I’ve used Dbol
only cycles before with no issues. A longer acting testosterone
such as Testosterone Enanthate or test Cypionate won’t
fully kick in until about the 2nd-3rd week.
I should also mention it is important to note, that even those who have gotten off steroids may still get stuck on them, cardarine sarm results.
Steroids with anabolic properties like testosterone, oxandrolone, and nandrolone are considered to be
safe. It causes a transient increase in liver enzymes, altering your LFTs.
I’m Baiza, a health and fitness enthusiast, bringing over
5 years of experience in creating science-backed content
focused on weight loss and gym fitness. With D-Bal, you may obtain all the muscle-building
effects of steroids without actually ingesting them. Thus, the same benefits as Dianabol can be achieved without the risk of severe side effects.
After four weeks of usage, you can anticipate improved athletic performance, including increased endurance,
power, and speed. Dianabol enhances the body’s oxygen-carrying capacity
and boosts red blood cell production, resulting in enhanced overall performance.
In this article, we will take a look at what you can expect
to see in terms of muscle mass, strength, and overall physique after 4
weeks of using Dianabol. We will also discuss some of the potential
side effects of using Dianabol so that you can make
an informed decision about whether or not it is right for you.
If you’re looking for an alternative to Dianabol,
there’s a stack we highly recommend checking out. Therefore, if you’re thinking about running a Dianabol cycle,
you need to know what to do. From there on, most people will gradually build their way up to the desired dosage,
which doesn’t necessarily have to be 50mg. As you can see, there’s a lot of reasons why an athlete would take
Dianabol. But it’s important to know that it’s not all
benefits and there’s a lot more to learn. Although there are a few positives linked with Dianabol use
in women, there are also some negatives to consider.
Its short half-life also entails that it quickly exits the system,
offering relative comfort for those who wish to clear it from their body swiftly.
The right balance can result in optimal muscle gain and improved strength without unnecessary complications.
Determining an appropriate dosage often depends on an individual’s body
weight, experience level, and overall health. It is
critical that one takes time to understand their personal
requirements, as this will significantly influence their experience with Dbol.
It is an oral steroid and has a short half-life, meaning it is
rapidly metabolized by the body. Therefore, it’s essential to
take Anadrol daily to maintain stable levels. Many users opt to
split their daily dose in half to further ensure consistent blood levels of the steroid, taking
one half in the morning and the other half in the evening.
In addition, testosterone enhances the effectiveness of Dbol while reducing its negative side
effects. The optimal dose will reduce the likelihood of unfavorable health effects, and choosing the correct
stack will make all the difference. These steroids may be used
in conjunction with dianabol Before and After 8 weeks pills to
achieve the desired effects. Winstrol, an oral and injectable steroid, is a popular choice among bodybuilders, mainly owing
to its ability to facilitate lean muscle growth while
promoting fat loss. Winstrol is generally utilized during cutting cycles when the aim is to achieve a
toned and defined physique.
Individual variability plays a significant role in the results
achieved with Dianabol after four weeks. Factors such as genetics, dosage, diet, training program,
and overall health can influence the magnitude and rate of progress.
It is essential to understand that while some individuals may experience
significant gains, others may have more modest results. After 4
weeks of use, you can expect to see a significant increase in muscle mass.
This is because Dianabol helps your body retain nitrogen, which is essential for protein synthesis.
Protein synthesis is the process by which
your body builds and repairs muscle tissue. Bodybuilders who utilize Dianabol or other anabolic steroids should have
regular checkups to monitor their heart, liver, and long-term testosterone function.
www.net-pier.biz · June 9, 2025 at 4:29 am
70918248
References:
what are oral steroids (http://www.net-pier.biz)
E-Hp.Info · June 9, 2025 at 5:44 am
70918248
References:
Real Steroid Websites (E-Hp.Info)
Buying injectable steroids online · June 12, 2025 at 10:15 pm
70918248
References:
https://fastpanda.in/2024/09/07/temosure-20-capsule-everything-you-need-to-know/
Clizak.com · June 14, 2025 at 1:08 pm
70918248
References:
none – https://clizak.com/boost-your-online-presence-our-top-digital-marketing/,
none · June 15, 2025 at 12:44 am
70918248
References:
https://atsu.com.ec/2012/12/08/aenean-laoreet-tortor/
Stephania · June 15, 2025 at 1:57 am
70918248
References:
online poker real money us (https://japanstours.com/nature-holiday-quotes/)
Https://Thegolfperformancecenter.Com/5-Elements-Blog/Distance-Is-Overrated · June 15, 2025 at 4:31 am
70918248
References:
None (https://thegolfperformancecenter.com/5-elements-blog/distance-is-overrated/)
Binance账户 · June 15, 2025 at 6:03 pm
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
ou acheter de la testostérone · June 19, 2025 at 12:20 pm
Ils sont tous formulés à partir d’ingrédients naturels et sont dépourvus de produits de synthèse toxiques pour l’organisme. De même, ils constituent la façon la plus sûre d’accroître votre drive, doper votre libido et donner un formidable coup de pouce à votre masse musculaire. Si vous êtes un sportif de haut niveau, ces produits constituent la façon la plus légale et la plus efficace d’accroître vos performances et d’obtenir de meilleurs résultats. Un booster de testostérone est un complément conçu pour augmenter les niveaux naturels de testostérone dans le corps. La testostérone est une hormone clé pour le développement musculaire, la libido et d’autres fonctions corporelles critiques. Les boosters contiennent souvent des ingrédients comme le tribulus terrestris, l’acide D-aspartique, et différents extraits de plantes. Certains prétendent qu’ils peuvent aider à compenser la diminution de la manufacturing naturelle de cette hormone avec l’âge.
Un ester d’acide carboxylique est élégamment intégré à une hormone synthétique de pureté remarquable. Testo enanthate peut être acheté en pharmacie ou testostérone enanthate vente en ligne. Convient aux débutants et à ceux qui prennent des stéroïdes depuis longtemps. L’énanthate de testostérone est l’un des stéroïdes anabolisants les plus populaires.
Il s’agit de l’option la plus puissante pour réussir à obtenir des résultats satisfaisants dans tous les aspects de sa vie (sport, santé, motivation…). La testostérone propionate aide à accélérer le métabolisme afin que vous puissiez brûler plus de calories, même au repos. C’est presque comme une forme de codage informatique pour les cellules musculaires.
Chaque ingrédient de PrimeMale a prouvé son efficacité dans de multiples études cliniques publiées dans des revues médicales et scientifiques reconnues. Les principaux ingrédients sont Tongkat Ali, Tribulus Terrestris, du Fenugrec et de la vitamine D3. Les utilisateurs ont signalé des changements radicaux dans leur corpulence et leurs performances sexuelles après juste quelques semaines d’utilisation. Au bout d’une période de three à 4 mois, la plupart d’entre eux ont connu une transformation complète de tout leur corps, un rehaussement de leur humeur et une motivation accrue pour entreprendre. Si vous remarquez des effets indésirables non mentionnés dans cette discover, ou si certains effets indésirables deviennent graves, veuillez en informer votre médecin ou votre pharmacien. Dans de rares cas, des tumeurs malignes du foie ont été observées après utilisation de substances hormonales telles que la testostérone. Votre fonction hépatique doit être contrôlée périodiquement par votre médecin.
Consultez nos catalogues, voici les hits du marché moderne, testostérone injection prix vous surprendra agréablement, automobile elle est problem de fabricants. En contactant des conseillers compétents, vous pouvez toujours compter sur une assistance pour choisir le produit adapté à vos besoins. Libonex semble être un complément alimentaire encourageant pour ceux qui cherchent à améliorer leurs performances sexuelles et augmenter leur niveau de testostérone. Avec des réductions intéressantes et une garantie de remboursement de 60 jours, il vaut la peine d’être essayé.
Il existe également des médicaments qui peuvent augmenter le taux de testostérone. Sur cette page, vous trouverez des informations sur les symptômes, les causes et les options de traitement d’une carence en testostérone. Performax est particulièrement recommandé aux hommes actifs physiquement qui cherchent à obtenir des résultats plus rapidement et durablement.
Acheter vos stéroïdes anabolisants injectables chez Pharmax-fr.com, c’est faire le choix de la qualité à un prix compétitif, avec l’assurance d’un service rapide et discret. Voyons à présent comme augmenter naturellement votre taux de testostérone pour rester au top de votre virilité, à l’aide de 5 composés naturels et efficaces. Dans tous les cas, le taux sanguin de testostérone diminue irrémédiablement avec l’âge, d’environ 1 à 2 % par an, et ce dès 30 ans. Des formules spécifiques sont d’ailleurs conçues pour accompagner les hommes de plus de 50 ans qui souffrent d’aromatisation de la testostérone. Ces effets secondaires rappellent qu’il est essentiel de respecter les doses recommandées et de ne pas chercher à “surcompenser” un déficit réel ou supposé. Tout complément ou traitement agissant sur la testostérone doit être envisagé avec encadrement médical, notamment par bilan hormonal régulier. Testo-Max se prend en cure de deux mois, à raison de 4 capsules chaque matin, 20 minutes avant le petit-déjeuner.
Vous pouvez acheter de la testostérone cypionate https://www.adgcf.fr/upload/pgs/acheter_de_la_testosterone.html énanthate, les deux formes les plus populaires. Les culturistes préfèrent souvent acheter de la testostérone injectable pour obtenir des résultats rapides et puissants. – La Testostérone améliore considérablement l’équilibre nerveux (chez l’homme uniquement), quand elle est prise sous forme de remedy de plusieurs semaines. Elle améliore le sommeil de qualité, et favorise un sommeil profond et réparateur, en sachant que le stress et des manques de sommeil diminuent considérablement la quantité de Testostérone dans le corps. Plusieurs études scientifiques récentes ont confirmé l’action de la Testostérone dans la meilleure gestion du stress, de l’anxiété, de la dépression, des peurs et des crises de paranoïa. En outre, l’utilisation de testostérone pour la musculation peut entraîner une dépendance psychologique, où les individus ont du mal à arrêter l’utilisation de stéroïdes anabolisants malgré les conséquences néfastes pour leur santé. Généralement, les injections de testostérone sont prescrites pour traiter l’hypogonadisme, un hassle caractérisé par des niveaux insuffisants de testostérone dans le corps.
Dexter · June 19, 2025 at 5:03 pm
Dianabol’s quick half-life (3–5 hours) means it ought to be dosed 2–3 occasions every day to maintain steady blood serum levels. Dianabol is a 17-alpha-alkylated oral steroid, which means it has been chemically altered to survive first-pass liver metabolism. Prolonged or high-dose usage can lead to elevated liver enzyme levels, liver strain, or even hepatocellular harm. While the benefits of Dianabol are impressive, it’s crucial to approach its use with a full understanding of the potential health risks and physiological consequences. As a 17-alpha-alkylated oral steroid, Dianabol is chemically modified to survive digestion and first-pass liver metabolism. While this makes it efficient, it additionally places vital stress on the liver, growing the danger of hepatotoxicity (Nieschlag & Vorona, Nature Evaluations Endocrinology).
Even probably the most revered and sought-after brands of Testosterone Enanthate from underground labs ought to be very inexpensive. This is one of the most inexpensive steroids we will use, leaving you with more money to spend on a few of the other dearer steroids that you just would possibly plan to stack with. You know you’re getting one of the best version if you can find Testosterone Enanthate at a pharmaceutical grade level. The greatest pharmaceutical-grade Testosterone Enanthate can additionally be anticipated to be the most expensive. With Testosterone Enanthate’s lengthy half-life, once you’ve had your last injection of the cycle, you should wait till that exogenous testosterone supply exits the system sufficient to stop shutting you down. One of the more notable variations is the oil in which the hormone is suspended.
You might experience fatigue, low libido, mood swings, and different potential signs. PCT should be began as soon as attainable after Dbol because this steroid has suppressive properties. This implies that remaining on Dbol can affect a person’s bodily features for a protracted time.
Extra superior testing strategies, similar to hair follicle tests, can detect use over even longer periods. In addition to SERMs, many users incorporate over-the-counter dietary supplements to support overall health and keep features during PCT. These may include testosterone boosters, liver support dietary supplements (given Dianabol’s hepatotoxicity), and common well being supplements like omega-3 fatty acids and multivitamins. Many customers report elevated urge for food while on dianabol without pct – https://jbhnews.com/dianabol-post-cycle-therapy-dosage-cycle-length-etc/29952/ -, which can be beneficial for those seeking to achieve mass however may lead to unwanted fat achieve if not correctly managed. The steroid’s impact on glycogenolysis can present elevated power and endurance throughout exercises, allowing for extra intense coaching sessions.
The pituitary gland produces HGH and influences bone and muscle development, amongst other capabilities. Though it could promote muscle development, it does so in numerous methods than anabolic steroids. Accurate testing for HGH in athletes just isn’t as simple as detecting most anabolic steroids or different PEDs, and urine testing cannot be used to detect HGH. A particular take a look at has been created to detect HGH in athletes, known as the Human Growth Hormone (hGH) Biomarkers Check, which focuses on detecting levels of IGF-1 and P-III-NP. Long-term threat elements are recognized simply because of our understanding of adjustments that top doses of HGH cause within the body. Kind 2 diabetes can develop when too much HGH is taken over lengthy periods.
Professionals are attempting to tailor help to AAS customers the place resources permit however few studies have explicitly asked users what type of support they want. There is doubtlessly numerous AAS customers who have not been surveyed as they are not accessing local substance use services or select not to complete surveys for fear of being categorised as ‘junkies’ [60]. Our search found several papers referring to query 1, but few regarding query 2, subsequently the search strategy was revised for question 2. Scoping reviews do not essentially need to rate the standard of the papers [27], nevertheless the authors concluded that due to the complexity of identifying participants, such a prime quality evaluation was of worth. Subsequently, for question 1, solely peer-reviewed documents were included to ensure a stage of quality, and this proved fruitful when considering assist accessed. One report that specifically sought info relating to best support wanted was recognized [33]. Acknowledging this report was not peer reviewed, the authors felt the data contained was of worth and related to the second question.
It can be like rolling a cube every time you buy Testosterone Enanthate from an underground lab, but that’s the chance we run when using steroids. Even essentially the most reliable suppliers can go unhealthy or disappear altogether with out warning. Underground labs check with manufacturing facilities that aren’t legally accredited and have no regulation or oversight of their practices. These labs can be something from professional-type facilities to a makeshift basement lab. You won’t know how or where your Testosterone Enanthate is being manufactured in underground labs or exactly what’s been put into it. This runs the chance of buying merchandise of poor quality and doubtlessly even dangerous Testosterone Enanthate if health and security measures haven’t been adhered to. Due to the link between high ldl cholesterol and high blood pressure, the latter have to be monitored while utilizing Testosterone Enanthate.
Proviron is taken into account a secure AAS, particularly in distinction to most different oral steroids, the place you might be used to worrying about liver toxicity and antagonistic effects on the kidneys. A newer SERM that has shown to be even more effective at restoring Testosterone (with fewer facet impact risks) is Enclomiphene. This is the SERM I use and suggest after most steroid cycles where Proviron is used in a stack.
growth hormone buy uk · June 23, 2025 at 9:07 am
Our team is committed to helping you achieve optimal well being and well-being via protected and effective HGH remedy. The greatest results will include treatments administered for months and generally years to optimise your body’s natural production of HGH ranges. Very quickly, performance-enhancing drugs (PEDs) grew to become the norm for bodybuilders and athletes who have been trying to push the limits of their our bodies. In one study, researchers discovered that in a 24-hour fast, the quantity of power your physique makes use of during numerous actions dropped, while growth hormone ranges rose by a lot. As A End Result Of the body’s HGH levels naturally lower with age, some so-called anti-aging experts have claimed that HGH merchandise could reverse the age-related decline of the body. The solely FDA-approved form of synthetic HGH comes as a shot, and you can get it solely by prescription.
At Verified HGH, our BPC-157 merchandise are manufactured to the highest requirements of quality and purity. When you choose to buy BPC-157 from us, you’re choosing a product that may effectively assist your therapeutic and restoration needs. Semaglutide is a peptide used within the treatment of type 2 diabetes and obesity. It capabilities as a glucagon-like peptide-1 (GLP-1) receptor agonist, which helps regulate blood sugar levels and promote weight loss. Earlier Than you purchase human progress hormone, it is worthy to understand the purpose of buying it. Alongside with that, you possibly can verify and see whether or not your requirements will be catered by the best legal human progress hormone that you purchase from us.
Some individuals use the hormone, along with different performance-enhancing medicine such as anabolic steroids, to construct muscle and enhance athletic efficiency. This consists of any possible unwanted effects not listed in the bundle leaflet. You also can report side effects instantly by way of the Yellow Card Scheme at /yellowcard or search MHRA Yellow Card in the Google Play or Apple App Store. By reporting unwanted facet effects, you’ll be able to assist present more data on the protection of this drugs. If you have any questions relating to the GroSupport programme, please speak to your healthcare skilled.
https://lamh.org.uk/wp-content/pgs/buy_hgh_38.html hormone is a 191-amino acid, single-chain polypeptide that is synthesized, stored, and secreted by somatotropic cells within the lateral wings of the anterior pituitary gland. Many factors influence the discharge of Human Progress Hormone, nevertheless, including diet and exercise. Human growth hormone on the market is prescribed for women and men who want to gently elevate and stability their development hormone ranges that have depleted with age. When blood work taken from a client reveals that their development hormone levels are depleted, accurately prescribed HGH injections might help.
The best choice will at all times be an HRT – hormone substitute therapy – specialist. Despite its high bioavailability, growth hormone supplementation could also be accompanied by some side effects. It is essential to consider these earlier than purchasing to observe your body’s response and adjust your course if needed. Free consultations with pharmacists are available through live chat on our website.
Understanding this distinction is essential in recognizing how MK-677 operates and its potential impact on the body’s hormonal system. HGH can speed up healing in the body, allowing for faster restoration following intense exercises. Weightlifting workouts designed to reinforce muscle mass trigger microscopic tears within the muscular tissues, which alerts them to repair and rebuild. Supplementing with HGH can facilitate faster muscle recovery, guaranteeing you’re pumping iron once more with minimal downtime. HGH dietary supplements can trigger lipolysis, your body’s own mechanism for burning fats. This motion aids in weight loss, enabling your body to melt away extra fat, even when you’re sleeping.
HGH is a naturally occurring hormone within the physique answerable for stimulating development, cell regeneration, and sustaining wholesome tissue. Athletes and fitness fanatics usually use HGH to speed up muscle recovery, improve power, and boost endurance. Additionally, HGH can assist in reducing body fat and improving pores and skin elasticity, making it a versatile solution for those targeted on well being and efficiency. Outcomes from using HGH can range depending on the individual and the dosage used. Typically, you might start to see enhancements in power levels, muscle mass, and general well-being within a quantity of weeks. Human development hormone, which is also referred to as HGH can deliver numerous advantages to you. If you are interested in experiencing these advantages, you can make the choice to go ahead and purchase HGH without having any second ideas in thoughts.
Boldenone Undecylenate can be successfully included in each slicing and bulking cycles due to the properly balanced results of this anabolic substance. Several components affect the price of a complete HGH routine, however patients can expect to pay between $1,000 to $5,000 a month for medically prescribed HGH. Her work ethic, fuelled by strong ambition, has driven her to turn into one of the revered private trainers of our era.
bewellprimarycare.Com · June 24, 2025 at 2:06 pm
By limiting testosterone in this cycle, Anavar is left to tackle the first anabolic function, bringing about lean positive aspects and unimaginable fat loss and firming throughout the cycle. More skilled users of Anavar often extend to the 50-70mg day by day dose whereas sticking to an 8-week cycle. A testosterone ester should also be included in an intermediate cycle, and once more, the dosage will depend upon what you’re making an attempt to achieve and whether this could be a hardcore chopping cycle. It can dry out your physique, promote unimaginable muscle hardening, and permit for a really dry, lean, and shredded physique best for contests or private targets. Ideally, you’ll be at a low body fats level before utilizing Anavar to take pleasure in its most physique enhancement effects.
Furthermore, the price of Anavar is very excessive, leading to fraudulent sellers reducing the volume of oxandrolone or eradicating it totally in change for a cheaper substance. People that purchase underground lab Anavar via the black market could claim doses of 15–25 mg per day are modest. This is due to copious scams the place the label states forty mg of Anavar, however in reality, it is only 20 mg.
As all the time, flexibility in adjusting your dose through the cycle is required. Since Anavar starts working shortly, you’ll have a good idea of whether or not you’re responding to this low dose early. Anavar additionally will increase nitrogen retention within the muscle17 – it is a prime operate of Anavar and is important in preserving the body in an optimum anabolic state.
Anavar will provide the capacity to build muscle and preserve power while dieting. Stacking Anavar will almost exclusively be for slicing and recomposition cycles for male users. Females will often use Anavar to realize lean mass, as ladies will be far more aware of the anabolic results of this steroid.
Cardiovascular exercise, or HIIT (high-intensity interval training), may be utilized to speed up a user’s metabolism whereas providing cardiac advantages. However, there are studies suggesting clenbuterol has muscle-building effects in animals (32). Clenbuterol’s anabolic potential stays controversial, with our sufferers and a lot of bodybuilders failing to experience any notable will increase in muscle hypertrophy throughout practical settings.
Keep In Mind, a robust assist community can be invaluable in your path to achieving your fitness targets. It is a premium-priced steroid, and you want to be prepared to spend some cash to get your palms on it. The value might vary depending on the supplier, the power of the drug, and your location. Nonetheless, be careful to not fall for suppliers selling Anavar at extraordinarily low costs as this could be a sign of pretend or counterfeited merchandise. In the Uk, Anavar is a managed substance and might solely be offered with a doctor’s prescription. This implies that selling Anavar without a prescription is in opposition to the law and can lead to critical authorized consequences.
Anavar however prevents muscle loss by significantly lowering cortisol (stress) levels. Anavar also slashes cortisol ranges, enabling you to burn fats from stubborn areas (lower abdomen). In recent years however the worth for anavar has dropped as a end result of it’s turning into easier to pay money for once more. We liv in a day and age now where with somewhat bit of analysis you possibly can merely go online and order some anavar straight to your home. It can be used to scale back muscle loss attributable to steroid use and to cut back bone pain in individuals with osteoporosis. It helps regain weight misplaced after surgical procedure, extreme trauma, or continual infections. Anavar for sale is also utilized by people who are unable to achieve or preserve a wholesome weight for unknown medical reasons.
In future Anavar cycles, 20mg could also be used from the 1st week onward; and the size of a cycle could also be increased to 8 weeks. It’s essential to notice that virilization side effects are rare in ladies (who use average doses of Anavar). And even when they did happen, they aren’t everlasting so as quickly as you cease taking Anavar; your hormones will steadiness out and these male characteristics are more likely to disappear. Some folks say they don’t notice much on anavar, which I put right down to a too-low dose.
Still, most girls will find that Anavar is extra well-tolerated in terms of controlling the side effects. For women who want to use Winstrol, the oral type solely is really helpful, and doses have to be saved very low to avoid virilization. If you have no existing kidney problems, using low doses and brief cycles of Anavar is unlikely to trigger kidney harm.
Anavar, also identified as Oxandrolone, is a popular anabolic steroid used by people trying to enhance muscle progress and athletic efficiency. If you’re considering buy Anavar UK, it’s essential to understand the process and ensure you make protected and informed selections. This guide will give you valuable insights into buying Anavar in the UK. Anavar UK, also referred to as Oxandrolone, has received outstanding popularity amongst UK athletes as a outcome of its specific perks and moderate nature in comparison with completely different anabolic steroids. When athletes select to buy anavar Online (https://bewellprimarycare.com/wp-Content/pgs/buy_Anavar_8.html) Anavar UK, they put cash into a performance-enhancing drug that provides great advantages with multiplied power, improved muscle definition, and improved endurance. However, like a number of substances used for athletic enhancement, it’s miles crucial to apprehend the right utilization, legal implications, and facet penalties of such dietary supplements. Anavar is often labeled as the most secure steroid for newbies, causing significant fats loss and noticeable lean muscle positive aspects.
wehrle.de · June 26, 2025 at 2:24 pm
Übergeordnet handelt es sich bei den Wachstumshormonen um die Progress Hormone (GH). Andere Bezeichnungen sind HGH, was human progress hormone bedeutet, oder Somatotropin (STH). Der insulinähnliche Wachstumsfaktor (IGF-1) ist das Ergebnis der vermehrten Bildung von Wachstumshormonen. Zwischen den Wachstumshormonen GH und dem insulinähnlichen Wachstumsfaktor IGF-1 kommt es zu einem Zusammenspiel mit zahlreichen Wechselwirkungen. Zusammenfassend lässt sich somit feststellen, dass HGH, GH oder Somatotropin (STH) das Gleiche meinen. Es geht immer um das Polypeptid, das als Wachstumshormon im Bodybuilding große Auswirkungen auf deinen Trainingserfolg und Muskelaufbau (https://wehrle.de/wp-content/pgs/hgh_kaufen_2.html) hat.
In seltenen Fällen können schwerwiegendere Nebenwirkungen auftreten, darunter Blutgerinnsel, starke Kopfschmerzen oder Sehstörungen. Sollten diese oder ähnliche Symptome auftreten, ist es wichtig, sofort einen Arzt zu konsultieren. Auch allergische Reaktionen wie Hautausschläge oder Atembeschwerden sind möglich, wenn auch sehr selten. Die richtige Einnahme von Progesteron Tabletten ist entscheidend, um die gewünschten gesundheitlichen Vorteile zu erzielen.
Sie sind Nahrungsergänzungsmittel, die ein anaboles Potenzial aufweisen und eine wertvolle Unterstützung für Sportler und körperlich aktive Menschen sein können. HGH Booster hingegen ist ein fortschrittliches Nahrungsergänzungsmittel, das die natürliche Produktion von Somatotropin, auch bekannt als Wachstumshormon, im menschlichen Körper steigern kann. Es ist eine Verbindung, die dazu beitragen kann, die Synthese von HGH im Körper zu erhöhen. HGH ist ein Polypeptid-Hormon, das aus etwa 191 Aminosäuren besteht. Es handelt sich um eine Substanz, die von den Zellen der Hirnanhangdrüse produziert wird und deren Ausschüttung unter anderem von Alter und Geschlecht abhängt. Das Nahrungsergänzungsmittel macht sich die Aminosäuren zunutze, um die menschliche Wachstumshormonproduktion in Ihrem Körper anzukurbeln und zu steigern.
Der menschliche Körper ist zwar in der Lage, Creatin selber zu produzieren, jedoch mit zwischen 1 und 2 Gramm nicht in ausreichender Menge. Um den täglichen Speiseplan besser zu optimieren, vertrauen viele Sportler aufs Trainieren und auf Supplements, die sogar sicherstellen, dass sich in ausreichenden Mengen, Nährstoffe im Körper befinden. Obwohl es immer besser ist, Muskeln auf natürlichem Weg auszubauen, nehmen viele Personen eine Abkürzung in Form von Anabolika. Was diese Mittel mit einem Körper machen können, ist nicht schnell aufzuzählen.
Die Dosen des HGH werden zur Vereinfachung der Messung in IE (Internationalen Einheiten) gemessen, da die tatsächlichen Milligramm-Messungen und -Konzentrationen sehr verwirrend und unpraktisch werden können. Dies bedeutet, dass eine einzelne Durchstechflasche mit 10 IE Human Progress Hormone 3, mg Human Progress Hormone enthält. Die Messung des HGH in Milligramm ist daher unzuverlässig und unpraktisch. Daher werden Messungen von GH-Dosierungen immer in IU-Maßeinheiten durchgeführt. Weitere Informationen zu diesem Thema der ordnungsgemäßen Rekonstitution, Lagerung und Haltbarkeit von menschlichem Wachstumshormon finden Sie in Kürze im Abschnitt zur ordnungsgemäßen Verwaltung dieses Profils. Eine übermäßige Zufuhr von Wachstumshormonen kann jedoch Symptome wie Gelenk- und Muskelschmerzen oder übermäßiges Schwitzen hervorrufen. Wachstumshormon-Booster sind Enhancer, die die natürliche HGH-Synthese im menschlichen Körper steigern sollen.
Mit den genannten Tipps, kannst du deinen HGH-Wert ziemlich einfach steigern. Das menschliche Wachstumshormon HGH hilft deinem Körper bei Stoffwechselvorgängen, Zellreparatur und anderen lebenswichtigen Funktionen im Körper. Wie bei allen anderen wichtigen Hormonen – wie Testosteron und Östrogen – ist es wichtig, einen gesunden Hormonspiegel des Human Progress Hormon (HGH) zu haben. Mehrere natürliche Nahrungsergänzungsmittel können die Produktion des Human Development Hormon vorübergehend erhöhen. Während schon ein guter Schlaf allein den HGH-Spiegel begünstigen kann, haben weitere Untersuchungen gezeigt, dass ein Melatonin-Präparat die Produktion des mesnchlichen Wachstumshormon HGH direkt steigern kann (35, 36, 37). Konzentriere dich auf die Optimierung der Schlafqualität und versuche 7-10 Stunden Schlaf pro Nacht zu bekommen. Ein erholsame Tiefschlaf steigert nachweislich die Produktion des Human Growth Hormon.
Progesteron spielt eine Schlüsselrolle im weiblichen Menstruationszyklus. Es wird nach dem Eisprung von den Eierstöcken produziert und bereitet die Gebärmutterschleimhaut auf die Aufnahme einer befruchteten Eizelle vor. Ohne ausreichendes Progesteron würde es zu Schwierigkeiten bei der Einnistung kommen, was die Fruchtbarkeit erheblich beeinträchtigen könnte. Bei Frauen mit Progesteronmangel können Symptome wie unregelmäßige oder ausbleibende Perioden, prämenstruelles Syndrom (PMS), oder eine schwierige Einnistung während der Schwangerschaft auftreten. Progesteron Tabletten helfen dabei, das Gleichgewicht der Hormone wiederherzustellen und Beschwerden zu lindern. Häufig kommen sie auch im Rahmen einer Kinderwunschbehandlung zum Einsatz, um die Gebärmutter auf die Einnistung der befruchteten Eizelle vorzubereiten.
Es verdoppelte auch die Spitzenleistung und erhöhte den HGH-Wert im Vergleich zur Kontrollgruppe. In einer Studie erhöhten four,eight Gramm Beta-Alanin vor dem Coaching die Anzahl der durchgeführten Wiederholungen um 22% (30). Einige Nahrungsergänzungsmittel können die Leistung optimieren und den HGH-Spiegel erhöhen. Andererseits kann Sport und Coaching auf lange Sicht deine Hormonfunktion optimieren und unnötiges Körperfett abbauen, was wiederum deinen HGH-Spiegel verbessert. Das Coaching bietet aber hauptsächlich kurzfristige Steigerungen der HGH-Werte. Der Anstieg hängt von der Art der Übung, der Intensität, der Nahrungsaufnahme rund um das Training und den körpereigenen Eigenschaften ab. Eine Studie ergab, dass die Einnahme eines GABA-Nahrungsergänzungsmittel zu einem Anstieg des Wachstumshormon HGH von 400% im Ruhezustand und 200% nach dem Training führte (27).
card Game · June 26, 2025 at 4:07 pm
Bidding is an important facet of Pinochle the place players estimate the variety of factors they imagine their partnership can earn. For example, going “nil” means bidding to win zero tips, whereas bidding a “meld” includes declaring particular mixtures of cards in your hand. The primary goal in Pinochle is to accumulate points by winning tricks. You win tricks by playing higher-ranking cards or strategically utilizing priceless cards to safe factors.
If you’re looking for a enjoyable and challenging https://blackcoin.co/two-handed-pinochle-poker-professional-tips-for-playing-and-winning/ to play with a pal, look no additional than Pinochle. This basic game has been loved by generations of gamers, and it’s simple to see why. With its distinctive scoring system and strategic gameplay, Pinochle is a recreation that rewards each skill and luck. If you’d prefer to play card games, but prefer something other than Pinochle, why not try our list of 10 simple and enjoyable card games? Or, if you don’t have anyone to play with, here’s a list of solitaire card video games.
Each participant is unbiased and competes in opposition to the other two gamers. Going clockwise, all players must comply with swimsuit unless they don’t have any playing cards in that suit. If you wouldn’t have a card in the lead go well with and you have a trump card, you should play the trump card. The highest card within the suit wins until a trump card is performed. If more than one trump card is performed, the best of the trump cards wins. Robert J Gauen stories a different technique of scoring frequently used within the Pacific northwest of the USA. Each team is allotted 14 colored chips (one group purple, the opponents blue) representing one hundred points each and 10 white chips representing 10 factors every.
The dealer shuffles the cards in whatever manner is convenient to combine them thoroughly. All gamers will play a trick, and the one with the very best scoring trick (trump always trumps) gets to go first on the subsequent round. After every trick, you draw a card from the deck to restore your total to 12. After dealing 12 cards to every participant (you’ll need multiple deck if you’ve obtained over three players), flip the cardboard on the top over; its suite would be the trump suite.
This is the place you and your partner can swap cards to enhance your hand. To take benefit of this chance, you should have a clear strategy in mind. The different gamers must then play a card of the identical go well with if they’ve one. Bear In Mind to concentrate to your cards in the course of the Melding Phase and attempt to kind essentially the most priceless melds possible.
Here, each player takes turns declaring a “bid,” which is an approximation of the variety of factors the cards in her hand might probably rating. The player who makes the highest bid (called the “contract”) wins the proper to declare the trump go properly with. The declarer leads the preliminary trick by enjoying any card they wish. You win a trick by taking half in either the highest-ranking trump card or, if there aren’t any trumps, the highest-ranking card that follows the leading go nicely with.
A Plain Marriage happens when you may have a king and a queen of any other suite aside from the trump suite, and that can get you 20 factors. Pinochle was born from a 19th-century French card sport often identified as Bezique, which itself was a by-product of a game known as Piquet. Bezique used to have the which means of “association” or “correspondence.” The English called this sport “Binocles,” which suggests “eyeglasses” (think of binoculars). A special observe — when bids are over 300, spades rely for double points. In Addition To making melds, there are two methods to score in Auction Pinochle — factors and bids.
When gamers play for tricks, there are strict rules which dictate what playing cards could be performed. Computerized variations enforce these guidelines programmatically. If the distinction between the amount bid and the quantity the declarer’s group has melded is 250 points or less, the hand could be played out. Basic courtesy requires all players to attend until the declarer picks up his or her own meld; then they may decide up theirs. This provides the declarer a fair likelihood to see what he or she is up against. There are loads of variations in scoring, bidding, and gameplay guidelines. When a trump is led, you should attempt to play a higher trump than the previous participant.
纸飞机电脑版 · June 27, 2025 at 9:19 am
Amazing article! I’ve Ƅeen searching for а reliable source tο
telegram下载 and
finally found oone that explains everything so cleaгly.
The content layout iѕ neat, aand Ӏ wass ale to get the telegram官网 link withⲟut аny
issues. you’re ⅼooking fоr telegram电脑版下载 or the latest telegram中文版下载, ths platform covers іt aⅼl.
Еven finding thе 纸飞机电脑版 wass effortless
here! Perfect fоr anyonne struggling witһ Telegram installation. Қeep up
the awesome wօrk — tһis reaⅼly helped mе geet what I
neеded!
Prihlásení · June 27, 2025 at 6:57 pm
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.
Lomba Prediksi · June 28, 2025 at 2:09 am
Every weekend i used to pay a visit this website, as i wish for enjoyment,
for the reason that this this web page conations truly fastidious funny material too.
https://ww5.jokermerah.city/
Bell · June 28, 2025 at 12:46 pm
70918248
References:
side effects of long term steroid use (https://codetrainee.com/articles/43)
Bob · June 28, 2025 at 4:46 pm
70918248
References:
pro bodybuilder steroid cycle (https://www.donmasivo.com/pregunta/cual-es-la-diferencia-entre-pampers-confortsec-y-supersec/)
www.cartergroupland.com · June 28, 2025 at 5:08 pm
70918248
References:
best steroid cutting cycle [https://www.cartergroupland.com/articles/land-spotlight-of-the-week]
https://bitpoll.de · June 28, 2025 at 7:18 pm
70918248
References:
most reputable online Steroid source (https://bitpoll.de/poll/5TCKBeachtennisOpen/)
https://talukadapoli.com/travel/listing/shahi-masjid · June 28, 2025 at 8:38 pm
70918248
References:
what is the safest Steroid for building muscle (https://talukadapoli.com/travel/listing/shahi-masjid/)
https://ap.multistyle.work/ · June 28, 2025 at 8:50 pm
70918248
References:
steroid forums sources (https://ap.multistyle.work/product/happy-ninja/)
https://vichiagro.Com/recipes/Recipe_Details/217 · June 28, 2025 at 11:06 pm
70918248
References:
steroids legal in usa (https://vichiagro.com/recipes/recipe_details/217)
https://whatfixedit.com/ · June 28, 2025 at 11:20 pm
70918248
References:
New steroid alternative (https://whatfixedit.com/question/ho-can-i-build-a-better-bond-with-my-dog/)
talukadapoli.com · June 29, 2025 at 1:12 am
70918248
References:
steroids for sale bodybuilding – https://talukadapoli.com/travel/listing/dreamland-inn-resort/ –
Is Animal Stak A Steroid · June 29, 2025 at 3:15 am
70918248
References:
https://talesofafrica.org/kenya-curbs-foreign-exchange-market-pressure-with-new-oil-deal/
techtunes auto · June 30, 2025 at 6:07 am
Thanks a lot! I appreciate it.
Daryl · June 30, 2025 at 3:21 pm
70918248
References:
steroids drug definition (https://shkolnaiapora.ru/question/raskras-razvyortku)
Williemae · June 30, 2025 at 5:10 pm
70918248
References:
where can you buy legal steroids (https://community.theclearwaytoconceive.com/question/the-10-most-scariest-things-about-best-robot-vacuum-and-mop/)
https://guardian.ge/ · June 30, 2025 at 5:12 pm
70918248
References:
steroids For runners – https://guardian.ge/66645-sri-lanka-president-gotabaya-rajapaksa-flees-the-country-on-military-jet.html –
https://office-nko.ru/dwqa-question/okazanie-uslugi-socialnoe-taksi/ · June 30, 2025 at 6:25 pm
70918248
References:
the adverse effects of Using anabolic steroids are serious because (https://office-nko.ru/dwqa-question/okazanie-uslugi-socialnoe-taksi/)