Learn the important differences between Ulcerative Colitis vs Crohn’s Disease. While both U.C. and Crohn’s are types of Inflammatory Bowel Diseases (IBD), they do have some important differences to know.
If you have recently been diagnosed with Ulcerative Colitis or Crohn’s Disease, or are suspecting you might be suffering with one of these conditions, this video / article will help you understand the similarities and differences between Ulcerative Colitis vs Crohn’s Disease.
As a bonus, you’ll learn one important tip regarding Ulcerative Colitis vs Crohn’s treatment.
Table of Contents
- Main Article:
Video:
Stream this Podcast episode:
Summary:
- Learn the similarities and differences between Ulcerative Colitis vs Crohn’s Disease.
- Learn how Ulcerative Colitis and Crohn’s are diagnosed.
- Understand 1 reason to be cautious about a particular type of treatment.
Main Article:
In this article, we are going to be discussing some of the major differences as well as similarities between Ulcerative Colitis vs Crohn’s Disease.
If you have recently been diagnosed with either Ulcerative Colitis or Crohn’s, or you are considering that you might be suffering from Inflammatory Bowel Disease (IBD), in which Ulcerative Colitis and Crohn’s are the top 2 “types” of IBD, then this video will help you get clear on what sets them apart and how they overlap.
I’m also going to be giving you one important tip when it comes to treatment for Ulcerative Colitis vs Crohn’s Disease.
Autoimmune Conditions / Chronic Inflammation
The first similarity for both U.C. and Crohn’s is that they are both considered to be autoimmune conditions at their core.
This means that the immune system isn’t functioning like it should. The body starts to improperly attack itself as if it is a foreign invader (like bacteria, a virus, or fungus).
This is what sets up and continues to cause chronic inflammation.
This is also why traditional anti-inflammatory treatments are not very effective long term. While you may be able to suppress the inflammation somewhat, you are not targeting the cause of the inflammation (the dysfunctional immune system) and thus the inflammation will continue to be produced.
While there are many different contributors / risk factors that can set the stage for the immune system to start the immune system from functioning improperly – such as genetics, diet [1], and chronic stress [2, 3] – there is no one trigger that is agreed upon to be THE cause.
Not “Overactive” Immune System – Dysregulated Immune System
It is important to point out that it isn’t really true that the entire immune system is “overactive” with Ulcerative Colitis or Crohn’s.
In fact, there are certain parts of the immune system, such as T-regulatory cells (a type of white blood cell), that are essentially always decreased in Ulcerative Colitis or Crohn’s.[4] This is important to know, because T-regulatory cells actually help protect our body from attacking itself.[4] Thus, decreased T-regulatory cell count actually increases autoimmunity (and thus chronic inflammation).[5]
Therefore, it is better to think in terms of immune system “dysregulation” instead of having an “overactive” immune system.
Besides T-regulatory cells, there are various other immune cells and cytokines that are either upregulated or downregulated in Crohn’s or U.C.[5]
Suppressing Entire Immune System Doesn’t Work Long Term
If we are locked into this idea that what we need to do is suppress the “overactive” immune system, then we might buy into the idea that repeated cortisone-like steroids is a good way to treat Ulcerative Colitis or Crohn’s.
However, many research papers have showed that this isn’t necessarily a good idea. While sometimes steroids can be effective short-term, when they are relied on long-term, they can create more problems than they solve.
For example, for Ulcerative Colitis, one paper states:
“Steroids may be temporarily effective, but subsequently may make patients steroid-dependent, resulting in long-term treatment and increased risks of adverse drug reactions. Therefore, it is important to withdraw steroids as early as possible in treatment of UC.“
Okayasu et. al. 2019
Similarly, for Crohn’s Disease, another paper states:
“Corticosteroids are highly effective in inducing clinical remission in patients with active Crohn’s disease. However, the role of corticosteroids in the treatment of this disease is primarily ameliorative because they are ineffective in maintaining remission or healing mucosal lesions. Nearly half of the patients who initially respond to corticosteroid therapy develop a dependency on corticosteroids or have a relapse within 1 year.”
Rutgeerts et. al. 2001
Understanding Inflammation and Healing
These results are easy to understand if you understand how the immune system works.
When you use steroids to suppress the immune system, you do temporarily decrease inflammation, but you also stop healing.
This is the same mechanism of how chronic stress (i.e. chronically high cortisol / stress hormones) can promote stomach ulcers.
The stomach lining is one of the tissues that need the most continuous repair. In fact, we get a new stomach lining approximately every 7 days or so. Therefore, if you are chronically stressed, and thus have chronically high cortisol, then healing and repair will be suppressed. For those without Crohn’s or U.C., the effect of this can show up first in the stomach as an ulcer.
For those with IBD, it can show up instead as a worsening / non-healing of their colon damage.
Again, this doesn’t mean that steroids should never be used.
It simply means they should not be relied upon long-term.
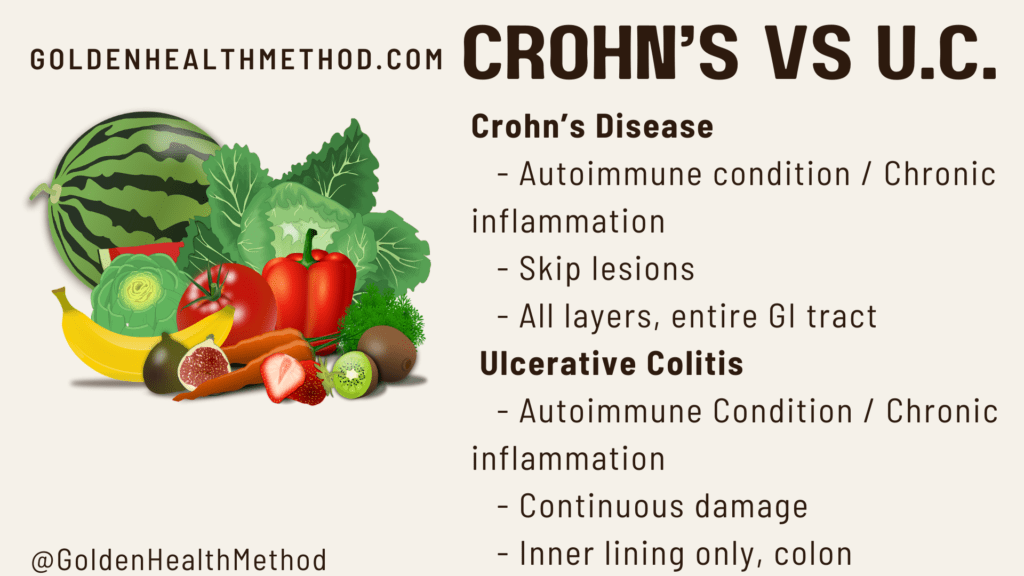
Ulcerative Colitis vs Crohn’s Disease: Different Types of Colon Damage
An important difference between Ulcerative Colitis vs Crohn’s Disease is the “type” of damage that gets produced and shows up during a colonoscopy.
In Crohn’s Disease, the doctor will observe something called “skip lesions”.
This is when there is damaged colon tissue, separated by healthy tissue, separated again by damaged tissue. Thus, the damaged regions “skip” around and are not continuous.
In contrast, for Ulcerative Colitis, the damage is more continuous throughout the colon. Skip lesions are not observed.
Ulcerative Colitis vs Crohn’s Disease: Different Layers and Areas of Damage
Entire GI Tract vs Colon Only
Besides the skip lesions, Crohn’s Disease can also affect more aspects of the gastrointestinal tract than just the colon.
For Crohn’s, the damage can actually appear anywhere from the rectum all the way to the mouth and lips. It can involve the entire GI tract. This is why sometimes those suffering from Crohn’s can develop mouth sores, for example.
This is in contrast to Ulcerative Colitis in which the damage is almost always contained to just the colon itself.
All Colon Layers vs Inner Layer Only
One last difference between Ulcerative Colitis vs Crohn’s Disease is that Crohn’s disease usually affects all the colon tissue layers.
For Ulcerative Colitis, usually only the inner layer of the colon tissue is affected.
Conclusion: Ulcerative Colitis vs Crohn’s Disease
I hope this helps you with your ongoing IBD journey!
Now you know about some of the major differences as well as similarities for Ulcerative Colitis vs Crohn’s Disease.
In an upcoming article, I am going to go over the differences and similarities in symptoms for Ulcerative Colitis vs Crohn’s Disease, so stay tuned for that; and if you haven’t subscribed yet to get updates, scroll up and click the subscribe button under the video above!
FREE GIFT
One last thing: If you haven’t yet enrolled in my new FREE mini-course “IBD: Get Your Fats Right“, you definitely will want to, because…
In it, I show you exactly why the types of fats that you are consuming can have a major impact on your disease and symptom progression. Most people underestimate just how important of a role fats play in IBD / Crohn’s / Ulcerative Colitis. By “getting your fats right”, you’ll be setting yourself up for some great IBD success!
This is NOT your generic “eat good fats, avoid bad fats”.
There is critical information in this course that I promise you haven’t heard anywhere else.
And it’s free, so check it out now!
Warmly,
Dr. Sean
References:
- Andersen V, Olsen A, Carbonnel F, Tjønneland A, Vogel U. Diet and risk of inflammatory bowel disease. Dig Liver Dis. 2012 Mar;44(3):185-94. doi: 10.1016/j.dld.2011.10.001. Epub 2011 Nov 3. PMID: 22055893.
- Sun Y, Li L, Xie R, Wang B, Jiang K, Cao H. Stress Triggers Flare of Inflammatory Bowel Disease in Children and Adults. Front Pediatr. 2019;7:432. Published 2019 Oct 24. doi:10.3389/fped.2019.00432
- Gao X, Cao Q, Cheng Y, Zhao D, Wang Z, Yang H, Wu Q, You L, Wang Y, Lin Y, Li X, Wang Y, Bian JS, Sun D, Kong L, Birnbaumer L, Yang Y. Chronic stress promotes colitis by disturbing the gut microbiota and triggering immune system response. Proc Natl Acad Sci U S A. 2018 Mar 27;115(13):E2960-E2969. doi: 10.1073/pnas.1720696115. Epub 2018 Mar 12. Erratum in: Proc Natl Acad Sci U S A. 2018 Apr 30;: PMID: 29531080; PMCID: PMC5879702.
- Pedros C, Duguet F, Saoudi A, Chabod M. Disrupted regulatory T cell homeostasis in inflammatory bowel diseases. World J Gastroenterol. 2016;22(3):974-995. doi:10.3748/wjg.v22.i3.974
- Yamada A, Arakaki R, Saito M, Tsunematsu T, Kudo Y, Ishimaru N. Role of regulatory T cell in the pathogenesis of inflammatory bowel disease. World J Gastroenterol. 2016;22(7):2195-2205. doi:10.3748/wjg.v22.i7.2195
- Okayasu M, Ogata H, Yoshiyama Y. Use of corticosteroids for remission induction therapy in patients with new-onset ulcerative colitis in real-world settings. J Mark Access Health Policy. 2019;7(1):1565889. Published 2019 Jan 22. doi:10.1080/20016689.2019.1565889
- Rutgeerts PJ. Review article: the limitations of corticosteroid therapy in Crohn’s disease. Aliment Pharmacol Ther. 2001 Oct;15(10):1515-25. doi: 10.1046/j.1365-2036.2001.01060.x. PMID: 11563990.







11 Comments
XMC.PL · May 2, 2025 at 11:13 am
The clarity and insight you offer here have the power to change the way we see the world around us.
types of injectable steroids · May 3, 2025 at 3:09 pm
They can be found in formulations such as ointments, lotions, lotions,
gels, foams, oils, options, and shampoos. The quantity of corticosteroid prescribed is dependent upon the period of
remedy, the frequency of application, the pores and skin location, and
the entire floor area handled. Sufferers may be taught utility using the fingertip unit methodology.
Anabolic steroids are a category of drug that mimic the effects of male intercourse
hormones known as androgens which stimulate muscle progress and secondary
male intercourse traits. They are sometimes abused by bodybuilders and other athletes to build muscle mass and so should be used
with warning. Corticosteroid medicines include cortisone, hydrocortisone and prednisone.
They are helpful in treating rashes, inflammatory bowel illness, asthma and other circumstances.
Rounding out the top three is methylprednisolone, which accounted for thirteen.4% of U.S.
steroid prescriptions and distributions final 12
months. Another steroid that is typically taken orally, methylprednisolone is used to
deal with extra severe conditions similar to blood issues,
lung ailments, and a few types of injectable steroids of cancer.
Like prednisone, the principle function of this steroid is to slow
down the immune system’s response to these various situations and reduce their subsequent symptoms.
This record is not full and many other medicine might affect Decadron. Decadron is
used to deal with many different situations such as allergic issues,
pores and skin situations, ulcerative colitis, arthritis, lupus, psoriasis,
or respiratory problems. Corticosteroids are produced within the adrenal gland positioned above the kidney.
This medication may trigger thinning of the bones (osteoporosis) or slow progress in youngsters if used for a very lengthy
time. Tell your physician in case you have any bone ache or in case you have an elevated threat for osteoporosis.
If your baby is using this drugs, tell the doctor if you assume your youngster
is not rising correctly. Although sure medicines shouldn’t be used collectively in any respect, in other circumstances two different medicines could additionally be used collectively even when an interplay might occur.
Most corticosteroids are available by prescription only (with the exception of over-the-counter nasal sprays or topical steroids
like hydrocortisone 1%). Corticosteroids were first used to alleviate symptoms of
arthritis back in 1948 at the Mayo Clinic in Rochester,
Minnesota. The drugs are synthetic versions of cortisol
produced by the adrenal glands, which connect to
the cortisol receptors on organs to elicit the
same effects. There are additionally behavioral treatments for substance use issues, such as contingency administration or cognitive behavioral
therapy. Corticosteroids are an important class
of drugs for treating all kinds of medical problems, including many inflammatory and autoimmune situations.
You may have to use these drugs for a number of months earlier than you get their
most profit. Injections of corticosteroids present a high dose of treatment
instantly into the affected joints. They may help cut back irritation within the joints and relieve pain, swelling, and stiffness.
Nonetheless, in certain situations, coming off
corticosteroids abruptly might be far more critical. This can cause
signs like very low blood pressure, decreased consciousness, and
seizures. This may be extra likely if another set off can also be present, like surgery or
illness. For gentle pores and skin circumstances, you would possibly take
an over-the-counter preparation, similar to one with hydrocortisone.
For others, you would possibly want a prescription-strength model, like Diprolene
(betamethasone dipropionate), however for much less than a restricted time (e.g., a
number of weeks).
Talk along with your doctor if you assume your baby isn’t growing at a traditional rate
whereas using this medication. You shouldn’t use this medication in case you are
allergic to prednisone, or when you have a fungal an infection that requires oral antifungal treatment.
Always consult your healthcare provider to make sure the knowledge displayed on this web page applies to your
private circumstances. If this side-effect occurs, it tends to
happen inside a few weeks of beginning treatment and is more
doubtless with greater doses. Sometimes individuals even turn into confused; they may develop delusional and
suicidal thoughts. If steroids are going to be taken long-term then it is usually advised to take medications or supplements
to strengthen the bones and help prevent osteoporosis.
Other forms of steroids embody lotions, ointments,
injections, inhalers and sprays.
You might need blood exams throughout most cancers treatment to
examine for this. Tell your doctor or nurse when you have headaches, nosebleeds, blurred or double vision or shortness of breath.
Feeling hungrier can make it troublesome to maintain your weight down. Your appetite will go back to regular whenever you stop steroids – however some folks need to diet to
lose the additional weight. Signs of an an infection embody a change in temperature, aching muscles, headaches, feeling cold and shivery and customarily
unwell. You might have different signs depending on the place the an infection is.
Steroids can disguise or change the indicators and symptoms
of some infections.
Skyrizi (risankizumab) is used to deal with plaque psoriasis,
psoriatic arthritis, ulcerative colitis … Otezla (apremilast) is used to treat plaque psoriasis, psoriatic arthritis, and oral ulcers …
Prednisone might improve your risk of harmful effects from a reside vaccine.
Live vaccines embody measles, mumps, rubella (MMR), rotavirus,
yellow fever, varicella (chickenpox), one type of the typhoid vaccine
and nasal flu (influenza) vaccine.
He additional describes his approach as science-driven, continuously
reviewing the most recent literature and concept. Danny ensures he has as many methods as attainable to assist folks enhance their
well-being and achieve their objectives. Exterior of work, he divides his time between family, basketball, and mountain climbing.
If Danny gained the lottery, he’d start a tech company specializing in deep studying to help individuals in coping strategies.
Though it has a legitimate medical use as a painkiller for end-stage
most cancers patients, this super-powerful synthetic opioid is more and
more showing up amongst fatal overdoses. In truth, throughout the previous three years, fentanyl-involved deaths
jumped by 540%.
closest thing to anabolic steroids · May 3, 2025 at 4:42 pm
They won’t produce long-term damaging results on a woman’s health, but they’re more doubtless to trigger virilization, probably affecting her long-term psychological
well-being. In reality, it stays one of many only steroids in research the place women can take megadoses of it
and nonetheless not expertise virilization. In one study, females got
as much as one hundred fifty mg per day for 30 weeks, and
none of them demonstrated any masculinization (3).
Female steroid use can be rife in sports, with girls
seeking to acquire an edge over their rivals and being tempted
by improved energy and endurance. Failed drug tests have haunted feminine athletes in sports activities corresponding to boxing, swimming,
CrossFit, and more. Anavar causes reductions in HDL ldl cholesterol, probably inflicting hypertension (high blood pressure) and increasing the danger of arteriosclerosis.
Nevertheless, in our lipid profile testing, Anavar only causes mild cardiovascular strain compared to
different anabolic steroids.
She followed it up with a top-five finish in the subsequent two editions of the show.
Garcia became a frontrunner to win the title when she scored a bronze
medal at the 2003 Olympia. Juliana Malacarne is the winningest Women’s
Physique Olympia champion of all time. She received the title for four-consecutive years between 2014 and 2017.
Sarah Villegas and Shanique Grant are tied for the second spot with two Women’s
Physique Olympia titles each. Bergmann received the lightweight division, whereas Murray bagged the heavyweight class and the general Ms.
Olympia title. The 2001 Olympia was the only 12 months in Ms.
Olympia history where the light-weight champ took the general
title.
None of them skilled a single concerning facet effect, except for
one girl wondering if possibly she had misplaced somewhat little
bit of hair (although she wasn’t sure). Two others mentioned
they experienced very gentle acne, which went away after the drug was discontinued.
One commonality between these girls is that have
been all first-time PED users. Being in a position to put that kind of
size on a lady in such a brief time period, without experiencing any masculinizing unwanted effects, is extraordinarily impressive.
While the official line from the pageant was
that these adjustments have been due to funds, many within the bodybuilding group doubted
this. In truth, some consider that the real cause was the rampant
use of steroids amongst feminine athletes. From overcoming
societal limitations to rewriting records, feminine bodybuilders have shattered stereotypes and
redefined what it means to be highly effective and female.
Let their stories function a beacon of motivation and a testament that greatness is within reach for each aspiring bodybuilder.
Setting the right dosage is crucial, as it can significantly impression the
effectiveness, security, and overall experience.
For a woman beginning her journey with Winstrol, it’s advisable to begin with a relatively lower dosage to provide a secure introduction to the substance.
As a rule of thumb, most females are advised not to exceed a daily dosage of 15 milligrams.
While dosages can differ based on private tolerance and health
objectives, greater amounts might increase the danger of experiencing opposed effects.
These can range from minor nuisances similar to oily skin and acne, to severe points like disruptions in menstrual cycles, voice deepening, and extreme body
hair development.
It is important to achieve success to counteract early fears
of not being adequate. A life-history with consuming disorders, bullying, unfavorable feedback
about look, lack of recognition, and lack of affection is frequent.
Three worked inside training or studied for jobs in that sector.
“One of the women stated this helped her to isolate herself and give attention to her training, job, work-outs and preparations for competitions,” says Havnes.
The stoppage of menstruation was an indication that the medicine have been effective.
The first is that he’s bringing to light a difficulty
in bodybuilding that nobody really needs to speak about.
Nonetheless, he did go to extra of the extreme than other bodybuilders, so this argument could not hold
up as well on situation that his routine and cycling was not the norm.
Bostin Loyd was simply 29-years old when he passed away on February 25, 2022.
With Out this deeper research, it additionally turns into harder to
have transparent conversations that would lead to needed modifications.
Scott Milne had some controversial legal issues in his lifetime,
with trafficking medicine and steroids, but the 6’3″ 250 lbs big-hearted large was nonetheless loved by the
bodybuilding community. Once you disrupt your natural hormones,
there is no guarantee that you’d ever have the power to bounce
again to your old self.
Throughout this time, some additional skilled shows were held, in addition to the three mainstays.
The 1994 schedule included the Canada Pro Cup, received
by Laura Binetti, and the primary of three annual Grand Prix occasions in Prague, gained by Drorit Kernes.
Besides offering the opponents with further opportunities to win prize money, these contests
also served as extra Ms. Olympia qualifiers. A new skilled contest, the Jan Tana Traditional,
was introduced in 1991. The contest was named for its promoter, a marketer of tanning merchandise, and ran annually
till 2003 with the departure of Wayne Demilia (it was later briefly revived in 2007).
The Jan Tana crammed the void left by the Women’s Pro World
contest, and occupied the quantity three slot on the professional circuit throughout its lifetime.
1991 also noticed Tonya Knight return to competitors, profitable the Ms.
Worldwide.
References:
closest thing to anabolic steroids
nordvpn coupons inspiresensation · May 6, 2025 at 7:07 am
This website was… how do I say it? Relevant!! Finally I’ve found something that helped me.
Many thanks!
Look at my web site: nordvpn coupons inspiresensation
tinylink.in · May 6, 2025 at 8:01 am
Awesome things here. I’m very happy to see your
article. Thanks so much and I’m looking forward to
contact you. Will you kindly drop me a e-mail?
Feel free to surf to my web-site – nordvpn coupons inspiresensation; tinylink.in,
easyurl.cc · May 6, 2025 at 1:03 pm
Very good article! We will be linking to this
great post on our site. Keep up the great writing.
Visit my website; nordvpn Coupons inspiresensation (easyurl.cc)
http://wall.sh/nordvpn-coupons-inspiresensation--47255 · May 6, 2025 at 1:58 pm
It’s amazing designed for me to have a website, which is helpful in favor of
my knowledge. thanks admin
My homepage: nordvpn coupons inspiresensation, http://wall.sh/nordvpn-coupons-inspiresensation–47255,
nord vpn coupon codes · May 9, 2025 at 9:50 pm
nordvpn 350fairfax
We stumbled over here by a different page and thought I may as well
check things out. I like what I see so now i’m
following you. Look forward to looking at your web
page yet again.
Here is my site nord vpn coupon codes
🔒 Email; TRANSACTION 1,963508 bitcoin. Withdraw =>> https://graph.org/Ticket--58146-05-02?hs=677fec32afc3d405dd8a0ab7f45334c5& 🔒 · May 11, 2025 at 5:22 pm
ib2kl0
JiliPH · May 14, 2025 at 1:10 am
Roulette strategies often fall short, but platforms like Jili777 offer a balanced mix of skill and luck with diverse casino games that keep players engaged beyond just chance.
Jili7 · May 15, 2025 at 5:36 pm
If you’re new to online slots, platforms like Jili777 offer a great mix of fun and smart play with AI features to boost your game. Definitely worth checking out!